Results (click for sub-categories)
Neutrophil Articles: A Table of Contents
StudyLTCOVID.com
Thanks for visiting!
To translate this page, select your
language from the dropdown menu below:
The six articles linked to below, relate to work with various aspects of neutrophil study, in those with "long-term" COVID-19 (LTC). They intend to introduce and present results of that work, and as developed throughout this site.
Some may find these, if not challenging reading, simply lengthy.
So to help with that possible impediment to extracting all that they have to offer, here is an interactive summary of their contents. This offers links to each article, and a résumé of the contents of each.
Here is a List of Abbreviations in what follows:
LTC - Participants with “long-term” COVID-19
NC - “normal” controls. Nothing to suggest acute or chronic SARS-CoV-2 infection nor any related symptoms
PBM - photobiomodulation. (an intervention with light fully developed on this site).
MS - multiple sclerosis
The goal here is to help present these White Blood Cells as more diverse in function, than simply gobbling up bacteria. The selected articles should help expand one's knowledge about neutrophils and their function in human health and illness. I think that for those with LTC, this is quite pertinent. That view is not too surprising, since I'm the one who did the research linked to below.
These results imply that measuring neutrophil size is doable, and provides results so obtained for LTC subjects. In that group, cell size at entry into the study, is markedly below that of NC subjects. Effects of brief exercise and PBM are presented in detail. PBM in LTC increases cell size, normalizing it. Exercise in LTC subjects, increases neutrophil cell size. Both these results are different from those in the NC group, and statistically distinct. The area of the body “targeted” for the PBM, and results obtained that relate to that variable, are also presented.
Morphology in Neutrophils - Brief Intro
The various components of “shape” are explained. Cell membrane shapes as “spheroidal,” “ovoidal,” and “ellipsoidal” are explained. The importance of including and emphasizing an image of differences related to location (intravascular, endovascular, or in the tissues) is emphasized, when considering potential differences in results.
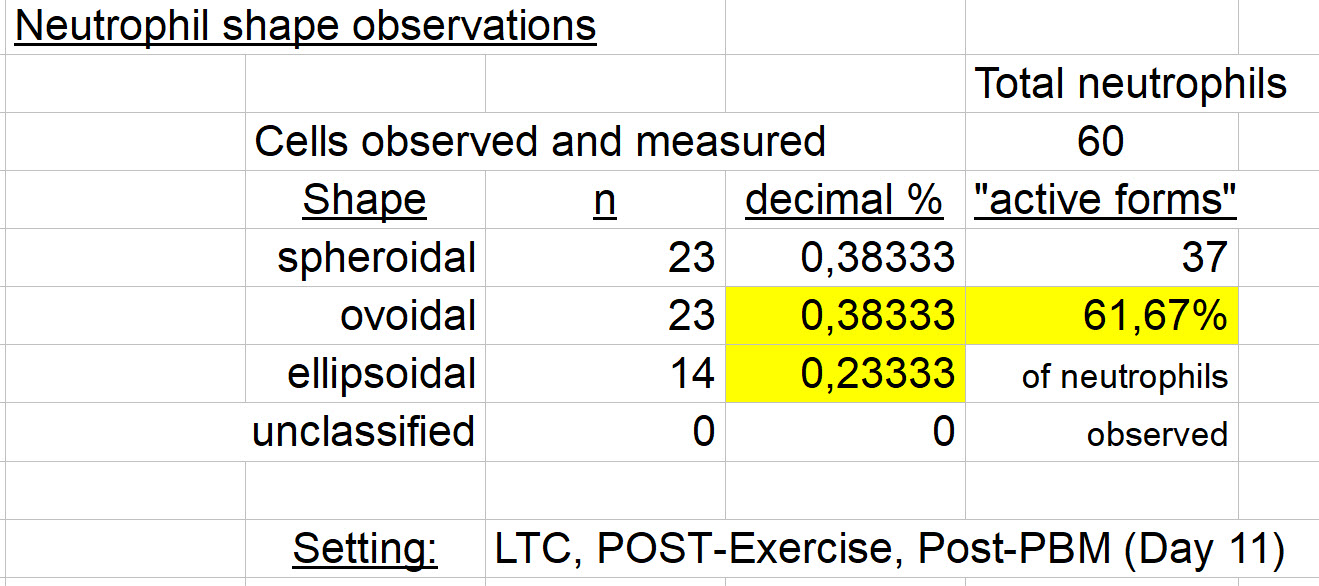
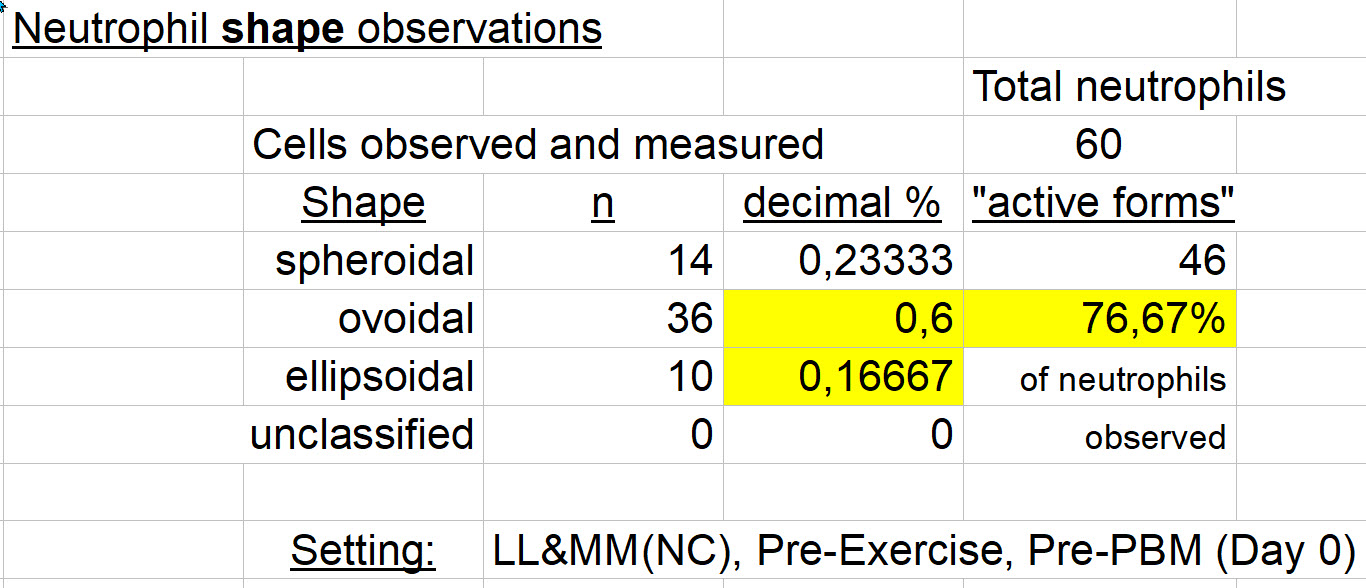
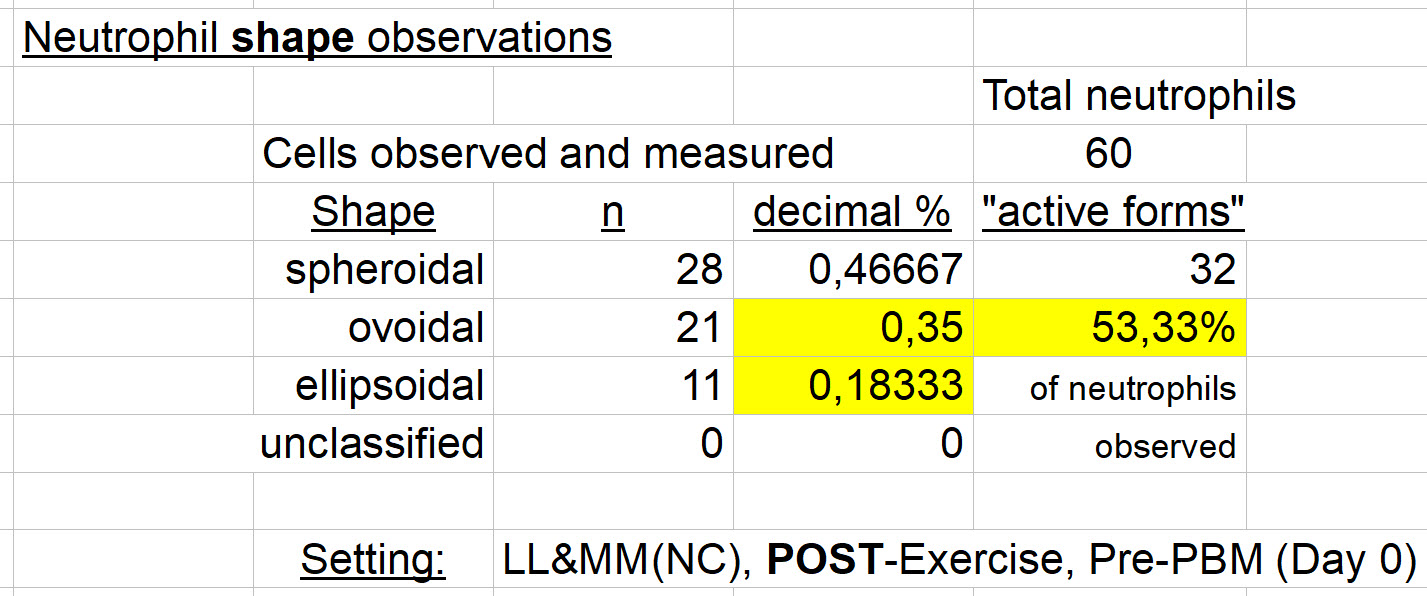
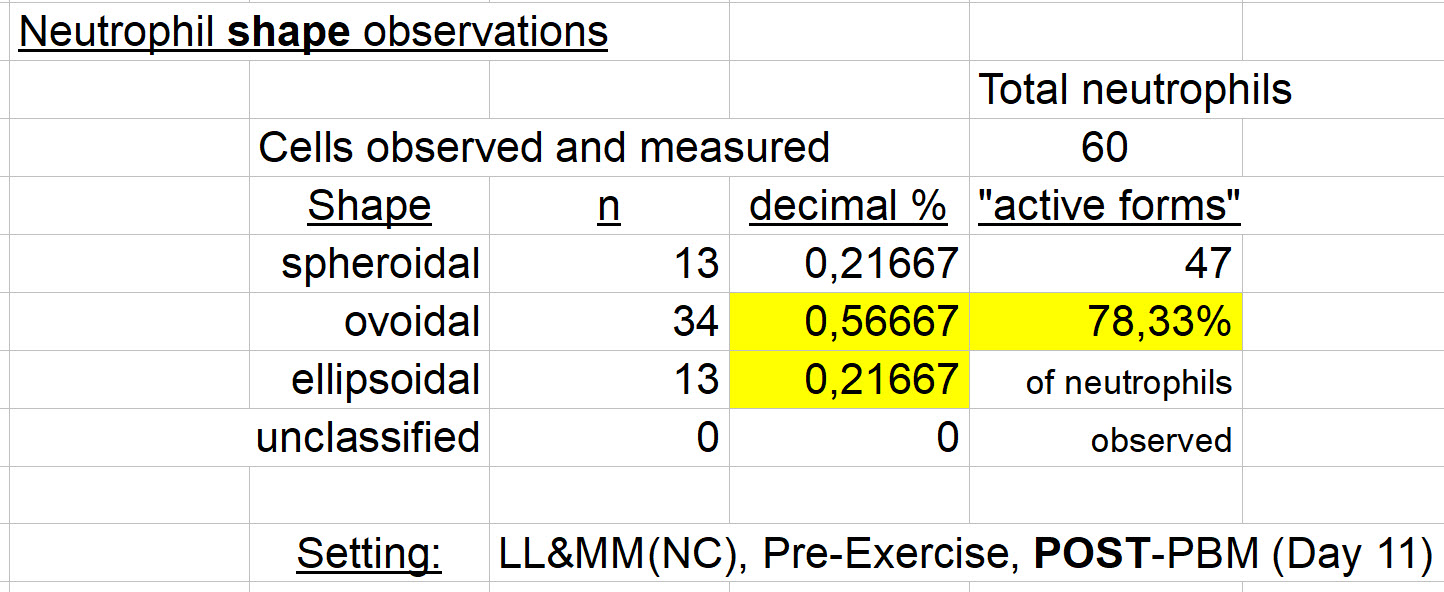
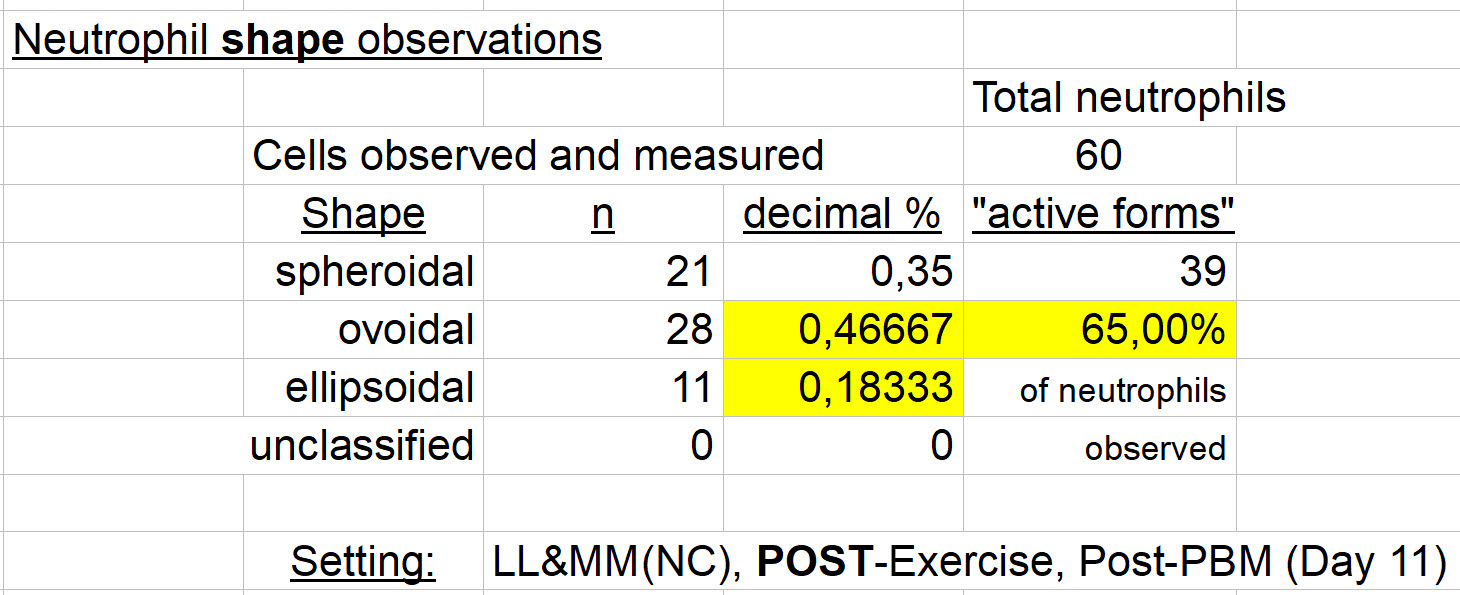
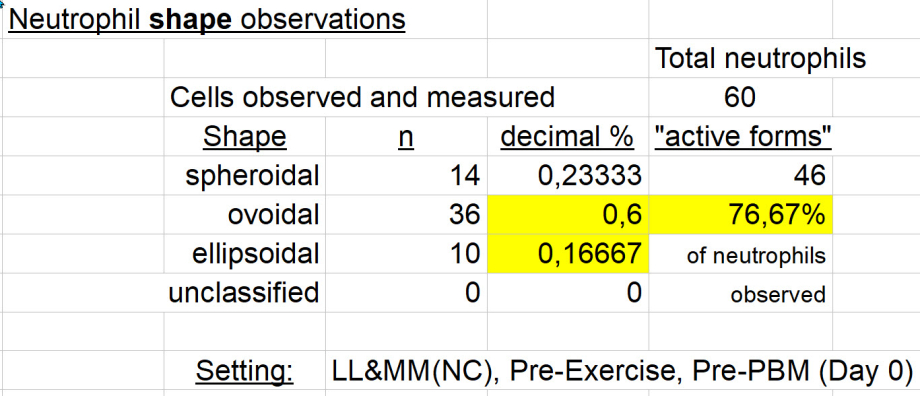
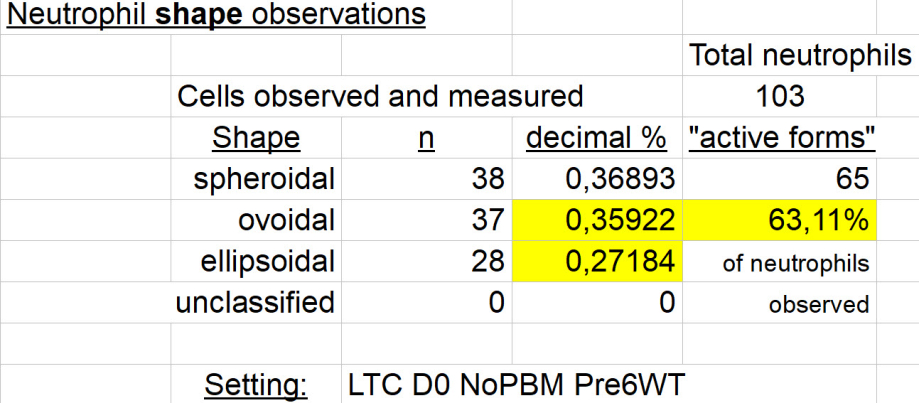
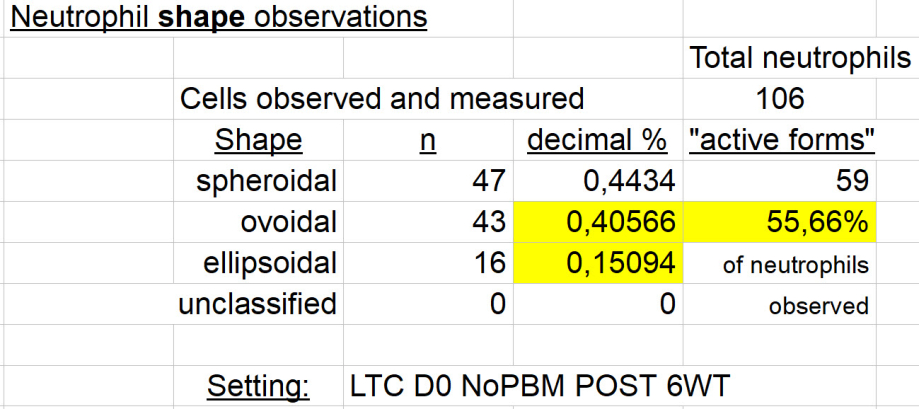
Neutrophil Cell Membrane SHAPE Observations
Another detailed comparison of neutrophils from LTC and NC subjects. Descriptions of "resting" or "on call," versus “active” cell mebrane forms are emphasized. Differences in cell membrane forms are identified Assumptions about importance of these differences are offered. Results and comparisons are presented to show that PBM in participants with LTC, normalizes cell membrane shape differences, as it did with size differences. Supportive statistical results are included. That transition in shape from "resting" to "active," is a process referred to in the literature as "priming" of neutrophils, followed by their "margination.". Some still unanswered questions are summarized.
------- presenting our study's work and results ends here -------
---- below, results from the related literature that are felt to be pertinent ----
Neutrophils & Multiple Sclerosis
|
The participation of neutrophils in the etiology, diagnosis, and treatment of multiple sclerosis (MS) is explored here. This, through links to 37 selected articles. Though this autoimmune disease, MS, is certainly ‘older’ than LTC, an understanding of the role of neutrophils is mostly still in an initiation phase for this illness. The articles express the logic of making this connection and pursuing it with additional research. At present, expressed positive findings have real, if newly discovered, importance. Many links to our work here with LTC should also come to mind. |
|
An exploration of the literature on this well-established anti-inflammatory plant-based alkaloid medication, and it’s ties to LTC and use in certain settings. While its use can be characterized as potentially beneficial and low risk, its use is not risk-free: As with almost all medications. Here, links to 47 articles may offer new and useful information. |
Neutrophils - Conclusions or New Directions.
When pouring over our results here, gets to be a bit too much, this may help.
Neutrophils
StudyLTCOVID.com
Thanks for visiting!
To translate this page, select your
language from the dropdown menu below:
On this page, several articles about neutrophils.
The goal here is to help present these White Blood Cells as more diverse in function than simply gobbling up bacteria, or forming Neutrophil Extracellular Traps (NETS) to capture such invaders.
I referred to this page in a presentation of results obtained from study of neutrophil size and morphology in negative controls, and subjects with "long-term" COVID-19 (LTC).
Other variables in that study included brief moderate exercise, and photobiomodulation as presented elsewhere throughout this present site. (See links below).
The selected articles should help expand one's knowledge about neutrophils and their function in human health and illness.
From one of these articles I cite some very basic but important information to carry through in one's readings on neutrophils:
"Neutrophils are short-lived (half-life 12±18 hr), postmitotic granulocytic cells that are produced in vast numbers (1 to 2 x 10^11 per day) in the bone marrow."
(from the S.Butcher et al. article on Ageing and neutrophil findings. Highlighting, mine).
The articles vary across several medical domains. But they all conclude that neutrophils have been too long ignored with respect to their heterogeneous nature and functions. Not only can each do more than gobble up bacteria to support our health. Their heterogeneity includes epigenetic responses that permit moving from one form and function to another within their short lifetime, usually measured in hours (18 to 36 hrs).
Moving through those articles that I selected, and here linked to, should help expand your thinking as it did mine. That is the goal for our purposes here, rather than presenting an exhaustive (and exhausting) review of the literature.
When articles are unavailable due to some restriction or subscription requirement, I try to place an ABSTARCT if avaialable, and as seen in what follows next below.
L.G., Ostuni, R. & Hidalgo, A. Heterogeneity of neutrophils. Nat Rev Immunol 19, 255–265 (2019). https://doi.org/10.1038/s41577-019-0141-8
“ABSTRACT
Structured models of ontogenic, phenotypic and functional diversity have been instrumental for a renewed understanding of the biology of immune cells, such as macrophages and lymphoid cells. However, there are no established models that can be used to define the diversity of neutrophils, the most abundant myeloid cells. This lack of an established model is largely due to the uniquely short lives of neutrophils, a consequence of their inability to divide once terminally differentiated, which has been perceived as a roadblock to functional diversity. This perception is rapidly evolving as multiple phenotypic and functional variants of neutrophils have been found, both in homeostatic and disease conditions. In this Opinion article, we present an overview of neutrophil heterogeneity and discuss possible mechanisms of diversification, including genomic regulation. We suggest that neutrophil heterogeneity is an important feature of immune pathophysiology, such that co-option of the mechanisms of diversification by cancer or other disorders contributes to disease progression.”
As one can sense from the titles, some are more general, and others pertain specifically to COVID-19 and its effects on myeloid cells (cells that originate in the bone marrow, and including neutrophils).
The articles vary in complexity, as the subject and results of each vary as well.
Good reading, at your leisure !
--------
Neutrophil chemoattractant receptors in health and disease: double-edged swords
The role of neutrophil death in chronic inflammation and cancer
Neutrophil diversity and plasticity: Implications for organ transplantation.
Neutrophil Diversity in Health and Disease
Strategies of neutrophil diversification
Current Understanding in Neutrophil Differentiation and Heterogeneity
Causes of variation in the neutrophil–lymphocyte and platelet–lymphocyte ratios: a twin-family study
A single-cell atlas of the peripheral immune response in patients with severe COVID-19
Global Absence and Targeting of Protective Immune States in Severe COVID-19
Severe COVID-19 Is Marked by a Dysregulated Myeloid Cell Compartment
"Basic" research at the lab bench
Clustered syk tyrosine kinase domains trigger phagocytosis
Myeloperoxidase-Halide-Hydrogen Peroxide Antibacterial System
Measuring Neutrophils ("Hey ! That's Us !")
Morphometry of human leukocytes
A Differential Role for Cell Shape in Neutrophil Tethering
A sensitive measure of surface stress in the resting neutrophil
Puzzle Pieces
Ageing and the neutrophil: no appetite for killing
Effect of age on human neutrophil function
Integrins: Bidirectional, Allosteric Sgnaling Machines
Neutrophils & Lactate
A separate page has been devoted to this important topic,
and is found at this link.
Window shopping
Congenital Defects in Neutrophil Dynamics
Evidence for macromolecular crowding as a direct apoptotic stimulus
>>> Neutrophil Size Changes - a study in those with LTC and Normal Controls (NC)
>>> Introduction to Neutrophil cell membrane shape changes
>>> Our neutrophil shape change results in NC and LTC subjects
Can neutrophil-related damage be moderated by other than PBM?
Here's one example that is pertinent:
>>> Lots of related info about Colchicine
And another:
>>> Neutrophils and Multiple Sclerosis
Neutrophil Size Observations
StudyLTCOVID.com
Thanks for visiting!
To translate this page, select your
language from the dropdown menu below:
The results presented here are paired to a presentation in June of 2024.
The topic: Observations and Comparisons related to neutrophil size measurements,
carried out previously on 1 796 neutrophils from several subjects.
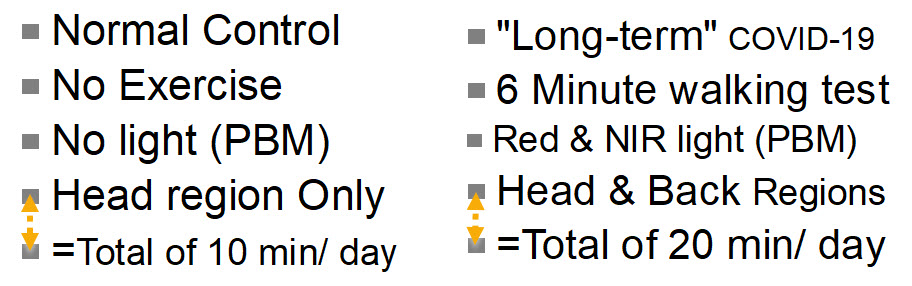
Variables that impacted on neutrophil size were given in that presentation, but include
For introductory and explanatory information, it is best to watch the actual presentation.
Information duplicated here allowed a more succinct presentation, while nevertheless providing access to observed results.
Here, the results of study, and as given in that presentation, will be repeated and summarized.
When comparisons have been made, observed differences are statistically significant unless stated otherwise. But the statistical values obtained from analysis of such comparisons of potential differences, will usually appear here as well.
It is important to emphasize that the samples are obtained by finger stick. That avoids problems with anticoagulants like EDTA as typically found in CBC tubes.
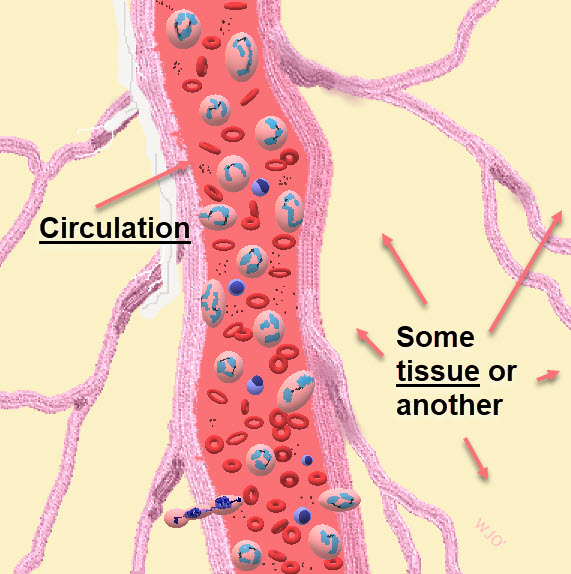
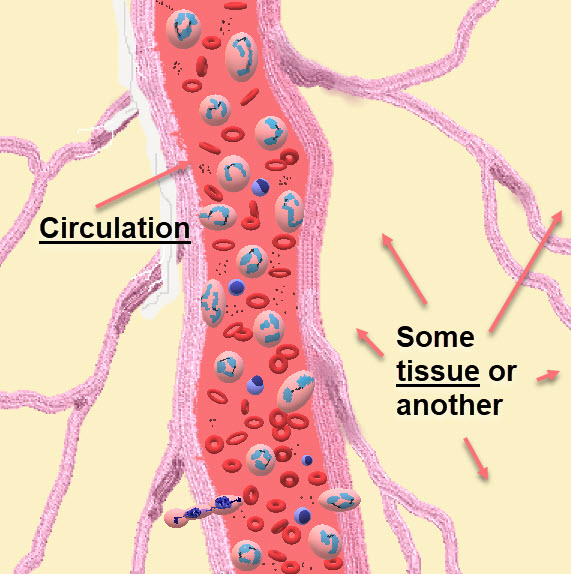
But what is the compartment of the body that is being sampled ?
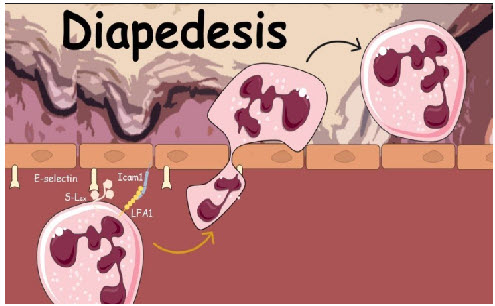
It is the vascular space. Adding to our message here, it is the intravascular space. So when numbers change and cellular areas decrease for example, consider the possibility that the larger cells have moved into a different space: a different extravascular compartment of the body. There, outside of the capillary, one finds the metabolic or immune "calls" that the neutrophils are responding to. So they leave the capillary (where they exist in one shape usually spherical), to adapt shape (ovoid & ellipsoid), to required response activities. This change in shape or morphology, permits movement in response to biomolecular calls to action.
In what follows, some results will seem close to giving the same message, but the goal here is sharing complete results of the study so far, and as promised in the presentation first referred to.
Before beginning ...
"Getting a little excited about neutrophils: is that a normal sort of thing?
They're in there somewhere. Theyre doing what they're supposed to be doing ...
But measuring them one by one.
Where does that interest come from?"
This may help answer that question:
"During moderate- and vigorous-intensity aerobic exercise
bouts of less than 60 min duration, the antipathogen activity of
tissue macrophages occurs in parallel with an enhanced recirculation
of immunoglobulins, anti-inflammatory cytokines, neutrophils, NK cells,
cytotoxic T cells, and immature B cells, all of which play critical roles in
immune defense activity and metabolic health."
"In general, acute exercise is now viewed as an important
immune system adjuvant to stimulate the ongoing exchange of
leukocytes between the circulation and tissues."
The above is selected from:
The compelling link between physical activity and the body's defense system
And if still not at all excited by any of this, maybe you just need to close this down and play a video game or something.
In Normal Controls (no COVID-19 ever, by History & Tests)
- Neutrophil size (area from two measurements) was about 150 to 160 µm²
- This is different than the commonly found "13.5 µm" diameter figure, found in the literature:
- Area = Pi x r², using a single maximal diameter measured with a light microscope, this well known equation overestimates size of ovoid and ellipsoid neutrophils by 15 to 20%.
- Our area results are from 2 perpendicular measurements of each cell.
- This is different than the commonly found "13.5 µm" diameter figure, found in the literature:
- In a negative control, (no COVID), before exercise, circulating neutrophils are 31% larger than those observed after exercise. Diff. in area: 47.11 µm² (no PBM involved here). Student's t-test, two-tailed: t = 7,7604; df = 58; p = 0,0001.
- In another negative control, (no COVID), before exercise, circulating neutrophils are 23% larger than those observed after exercise. Diff. in area: 35.8 µm² (no PBM involved here). Student's t-test, two-tailed: t = 4,4351; df = 58; p = 0,0001.
- Same negative control individual (No COVID) AFTER 10d PBM, brief moderate exercise (6'Walking Test) after 10 days of PBM to head region is associated with a significant reduction (-15.3%) in circulating neutrophil cell size. Difference in Mean size: 24,5 µm². Student's t-test, two-tailed: t = 4,4351; df = 58; p = 0,0001. (Same finding as before PBM, smaller cells after exercise).
- Same negative control individual (No COVID) BEFORE & AFTER 10d PBM, brief moderate exercise (6'Walking Test) on each Day 0 and Day 11. There is no significant change in neutrophil size (difference in Means: 2,66 µm², a diff. of 1.97%). Student's t-test, two-tailed: t = 0,4871; df = 58; p = 0,628 (N.S.) So exercise was again associated with reduced neutrophil size, but doing 10 days of PBM to Head Only, did not seem to impact this effect of exercise.
- In 2 Negative Controls (No COVID) AFTER 10d PBM, before exercise, circulating neutrophils are again 23% larger than those observed after exercise. (Suggesting: No additional PBM effect on cell size, to further modify the exercise effect in "normals"). Diff. in area: 35.9 µm². Student's t-test, two-tailed: t = 7,2998; df = 118; p = 0,0001
In a subject with Acute COVID-19, compared with her pre-infection, Pre-COVID-19 neutrophil cell size
- Below, a "highlights" video (shorter and faster) from 15-10-22 peripheral smear
- This is before any known viral contact or infection, or positive test, asymptomatic
- Below, a "highlights" video from 29-05-24
- This is after an infection on 17-01-24 which generated in the days that followed, mild symptoms and positive antigen tests for SARS-CoV-2
- Note that some of the cells captured here are not neutrophils but lymphocytes and others, included for size comparisons.
The above videos may give you a sense of how such measurements proceed.
But to say that the post-SARS-CoV-2 infection period is associated with any changes at all in this subject, would be most challenging. Any impression of any differences in size would be hard to confirm.
So allow me to add a statistical look at the pre- and post- COVID-19 findings in this single individual:
A reminder: in this article, cell size is being presented. Changes in form (morphology) are found elsewhere.
So if one still prefers measuring size of neutrophils as the largest diameter on a sphere:
- PRE-Infection size: 16.064±1.468 microns (n=32)
- POST-Infection size: 13.554±1.767 microns (n=37)
- significant difference in size (2.51 microns smaller on average) ?
- Student's two-tailed t-test: t = 6.3575; df = 67; p<0.0001
- In words: after an acute SARS-CoV-2 illness, neutrophils are significantly reduced in size
- but by this method, still "normal in size (=13.5±0.75 microns)" Z-score = 0,072
Using our two-dimensions method:
- PRE-Infection size: 174.410±23.069 µm² (n = 32)
- POST-Infection size: 129.877±23.567 µm² (n = 37)
- that's a 25.53% reduction in neutrophil mean size in this individual
- significant difference in size (44.53 square microns smaller on average) ?
- Student's two-tailed t-test: t = 7.9044; df = 67; p<<0.00001
- In words: after an acute SARS-CoV-2 illness, neutrophils are significantly reduced in size
- using this preferred (two-dimensions) method for neutrophil area, comparing with a normal value of (155.917±24.231 µm²), Z-score = -1.07466
- which simply means that this method discovers a reduction in size of about 1 standard deviation below the mean. The method above (single diameter), identified no such difference.
- using this preferred (two-dimensions) method for neutrophil area, comparing with a normal value of (155.917±24.231 µm²), Z-score = -1.07466
- Some will conclude that this point is just being fussy.
- As we'll see below, those with "long-term" COVID-19 sampled here, present with a marked reduction in neutrophil size.
- So perhaps here, a "transition period" or initial effect is being observed.
- This subject never developed (as of 07-07-2024) any symptoms to suggest a prolonged illness after her viral infection on 17-01-24.
- Eventually, a follow-up estimation of neutrophil size in this individual, will be performed to see what information that may add.
In this Acute COVID-19 subject compared with "Long-term" COVID-19
- Acute POST-Infection size: 129.877±23.567 µm² (n = 37), as given above
- as just shown, a significant reduction in size from her "normal" pre-infection value.
- Those presenting with more chronic illness: 88.198±28.758 µm² (n = 103)
- even without any statistical aide, clearly a difference.
- Diff. = 41.679 µm² or 32.09% smaller in the chronic illness group.
- A further reduction in neutrophil size in moving from acute to chronic illness. (t = 6,5219; df = 65; p = 0,0001 by Student's two-tailed t-test) is strongly suggested.
In those with "Long-term" COVID-19 (LTC)
- In subjects with LTC, brief moderate exercise (6'WT) is followed by a significant 26.3% INCREASE in size of circulating neutrophils. (before any PBM): A result opposite that of controls. Diff. in area: 23.2 µm². Student's t-test, two-tailed: t = -5,0335; df = 207; p = 0,0001. (A negative t-test value just indicates that one group's value obtained was smaller than the other. Many statisticians will always report 't' as a positive value).
- In subjects with LTC, brief moderate exercise (6'WT) after 10 days of PBM to head or head & back, is followed by a 14.1% increase in size of circulating neutrophils. A result again opposite that of controls. Diff. in area: 18.9 µm² Student's t-test, two-tailed: t = -4,0123; df = 219; p = 0,0001.
- Comparing the two results above: 26.3% - 14.1% = 12.2%. Meaning ? Whatever is causally associated with this finding, that is still different and opposite to that in controls, PBM in LTC is associated with a 12.2% "rapprochement" or reconciliation or normalization of that difference in size. Is that a statistically significant finding?
- By Chi² = chi-sq. = 9,79049; p = 0,0018. So while 12% may not seem to be a large difference, the 422 neutrophils observed generated a result that says that this is nevertheless a significant movement towards "normalization." A very significant difference in Exercise findings after 10 days of PBM: based on Neutrophil Morphology in LTC (p = 0,0018). This in support of the idea of a movement towards normalization linked to PBM in the LTC study subjects' cells.
- Just a thought: If in observing neutrophil shape one takes "speroidal' cells as cells 'in waiting', and "ovoid & ellipsoid" cells as those 'ready for action' in response to a "call" from the tissues, why can't these more active forms get out of the capillary to respond to the metabolic and immune "calls" ?
- Pericytes are specialized cells that wrap around and ensheath microvessels, promoting endothelial cell junction stability and depositing extracellular matrix (ECM), among many other key functions. In LTC, have they been damaged so that "active" neutrophils can no longer leave capillaries to get out into the tissues, thereby increasing in number in the circulation? Are the protective "tight junctions" now too tight ? Just a thought, not to say a hypothesis.
- The topic of cell membrane morphology (shape) in these studied neutrophils, in distinction from size, is introduced here, and results of measurements are covered in a different article, found at the link. Too much to include here.
- Comparing the two results above: 26.3% - 14.1% = 12.2%. Meaning ? Whatever is causally associated with this finding, that is still different and opposite to that in controls, PBM in LTC is associated with a 12.2% "rapprochement" or reconciliation or normalization of that difference in size. Is that a statistically significant finding?
- Comparison of LTC subjects with Normal Contols. No exercise in either group. No PBM in either group. (Referred to as 'Day 0'). Circulating control group neutrophils on Day 0 are 43.4% larger than circulating neutrophils from LTC subjects. A Mean Difference in cell surface area of 67.72 µm². This difference, before any PBM and independent of exercise. (A huge difference). Student's t-test, two-tailed: t = 15,3375; df = 161; p<< 0,0001).
- Compared with Negative Controls before exercise or PBM, LTC subjects' circulating neutrophils AFTER exercise have increased in size but remain significantly (14.92%) smaller than Pre-exercise controls. Student's t-test, two-tailed: t = 5,101; df = 148; p = 0,0001.
- Another go at this: Contrary to Controls, where exercise reduced circulating neutrophil size, in LTC subjects, size of circulating neutrophils increased significantly: 10.4% above post-exercise mean size of neutrophils in Controls. Student's t-test, two-tailed: t = -2,6869; df = 148; p = 0,008.
- In LTC subjects, exercise before and after the 10 days of PBM, was still assiociated with a 36.8% increase in circulating neutrophil size (LTC: PBM + 6'WT). Student's t-test, two-tailed: t = -7,4812; df = 220; p = 0,0001.
More results to follow for the LTC Group. And especially, morphology changes related to levels of neutrophil "activity" or "resting state" to use those terms here.
That article on morphology (shape) changes in LTC and Control neutrophils, is found at this link.
In the meantime, here is a link to another page on this site, and presenting articles about the heterogeneity of neutrophil form and function. They do more than just gobble up bacteria.
But if something interferes with their ability to move from capillary to tissue by diapedesis, and on demand, that will spell trouble. See the above link, repeated here, for results and a full discussion.
Exposure size: Head Only (10 min/d) or Head & Back (20 min/d)
In early 2020, well after the pandemic had begun, a questionnaire was formulated to obtain more information. The goal was to characterize what the "long-term" COVID-19 illness was like for those unfortunate enough to have it. As a separate entity, and as most recall, LTC was just emerging at that time. Estimates varied as to its prevalence, and much information has appeared since those earlier days of the (still ongoing) pandemic.
The work at that time, and the results of that first survey can be found at LTCOVID.com which was created and used to organize that initial effort. To help direct one's review of the observations presented on that site, here is a link to an Index of the Questions and their Answers, organized by question number (there were 60).
I start this section on "targets" for intervention using PBM, with a return to the past, for the following reason: to share what was learned that guided further study.
- As most now know, the initial response of the Medical System to those with LTC was much less than satisfactory. One such example, and covered in the survey mentioned above, was that anyone presenting with list in hand to more efficiently recall 16 physical symptoms, and 7 emotional symptoms must simply have an anxiety disorder which should be treated as such. Written reactions to such 'compassionate care' received at that time, can be found at Q.59 of the survey. Such 'care' and reactions to it, are still all too often (sadly) in evidence today.
- This also frequently contributed to heatedly presented responses to this bad care, and that argued strongly that this is a real physical illness, with physical manifestations and findings, and "can we please just drop the psychologic approach, and anxiety medication ?!"
- Nevertheless, the truth about a physical illness having an emotional component as observed in that survey (Q42, 43, 44) was neither surprising (a patient with appendicitis experiences one or more emotional components of that illness), nor has it just 'gone away' since those early days.
Those specific responses to the questionnaire helped define an approach to "targets" for the PBM intervention.
- Accepting (without surprise) that there were emotional components of this illness, and without forgetting nor minimizing the simultaneous physical findings, meant:
- we should "target" the head. That's where emotional issues are felt to live.
- that, without ignoring the relationship with the rest of the body, but
- that's where "emotions" are placed in our society
- if we were in a different or older society, the "target" might have been the liver or the kidneys, as the logical place for where emotions dwell and manifest from.
- the discovery that our devices for PBM emit a light that can penetrate into the head was supportive information.
- in a spirit of devotion to scientific method, the thought also occured that as long as you shine the light on the skin somewhere, that may be all you need, to address overall findings in those with LTC. The head has skin (usually), but let's add a little more skin surface to see what that does: was the thought at the time.
- so appeared as a "target": the back. Or the two: Head & Back.
- we should "target" the head. That's where emotional issues are felt to live.
Would shining the light on skin, no matter where on the body, still get a positive response, and including for that sticky issue (more or less accepted) of "emotional issues" ?
All of that needed to be embarked upon, not with sort of a "Whack-A-Mole" approach, but couched as well as possible, in all of the supportive Science. Here's an example of what's meant by "supportibe Science":
Estimation of the spectral absorption of light by components of human skin
Or,
Differences in light wavellengths and body penetration as carefully studied in that article.
Or,
Skull and vertebral bone marrow are myeloid cell reservoirs for the meninges and CNS parenchyma
The above reference gives new support for "targetting" the skull (head, in common usage).
I mean, one reason to "target" anything in this work, is to help a specific area that is theoretically involved with its presumed "problem." But what if there are mechanisms that permit neutrophils, for example, to be "targets"?
After all, they pass through the skin's capillaries.
After all, they travel everywhere.
And after all, in their travels they communicate with many other components of our innate immune system.
And of course, other pertinent reports, and as already presented back at LTCovid.com
One page where that was explored is found at this link.
Many other links at LTCovid.com, to published related works, can still be found and have not lost importance or relevance in the recent past years.
It will be mentioned here that if "Head Only" versus "Head and Back" made no difference, we accepted that 10 minutes per day, or 20 minutes per day might make a difference. That has yet to be explored; still a "thing to do" in our several protocols.
Back to the present
The evolution beyond that first work, initially and still today, can be found at several locations on this present site of StudyLTCovid.com, and for example: Interventions
The process described there, while still valid, has also evolved.
So we did all of that, and here are some of the results that emerged, and pertaining to neutrophil cell size and body part(s) exposed ...
In LTC subjects, exposing Head Only (so, 10 minutes/ day)
Results independant of any exercise were that Mean Neutrophil Size increased from 111.73±25.2 µm², n=43 (Day 0, Pre-PBM) to 138.73±31.2 µm², n = 45 (Day 11, Post-PBM). That difference, an increase of 27 µm², was statistically significant by two-tailed Student's t-test (t = -4.4547; df = 86; p=0.0001).
If the desired effect is to see an increase in neutrophil size in response to PBM in the setting of LTC, exposing Head Only is adequate.
In LTC subjects, exposing Head & Back (so, 20 minutes/ day)
Results here, are again independant of any exercise. Mean Neutrophil Size increased from 71.34±16.9 µm², n=60 (Day 0, Pre-PBM) to 129.69±26.4 µm², n = 60 (Day 11, Post-PBM). That difference, an increase of 58.35 µm², or 81.8%, was statistically highly significant by two-tailed Student's t-test (t = -14.4513; df = 118; p<<0.0001).
Exposing Head & Back and for twice the duration of the Head Only subjects, did increase neutrophil size.
In LTC subjects, which "target" size and duration was better?
Comparing the above results, and summarized as a Day 11, Post-PBM value for Mean Neutrophil Size of 138.7µm² in the Head Only/ 10 min group, with that of 129.7µm² in the Head & Back/ 20 min group, that difference was not significant (t = 1.6067; df = 103; p=0.1112).
While some might say that difference is quite close to being significant, the "smaller effort" may still be adequate to the goal when one is focused on increasing neutrophil size.
A reminder: Neutrophil size is taken as reflecting a cell's energy stores and response to metabolic needs, in varying states of health or illness.
An additional comparison that may be informative, even if presented above ...
In NC (normal, or Non-COVID Control) subjects, exposing Head Only (so, 10 minutes/ day) x 10 days
Results still independant of any exercise, Mean Neutrophil Size was 155.92±24.2 µm², n=60 (Day 0, Pre-PBM), and 154.03±21.7 µm², n = 60 (Day 11, Post-PBM). That difference, (essentially, no difference), was not surprisingly statistically insignificant by two-tailed Student's t-test (t = 0.4505; df = 118; p=0.6532).
Or perhaps simply put: What was normal, stays normal.
Other variations on the theme ... exercise effects, without any PBM
In LTC subjects, before any PBM, so independent of eventual "target" area and exposure duration (Day 0 at rest, then 6 minute walking test)
Results now reflecting only exercise effect: Mean Neutrophil Size pre 6'WT 88.198±20.76 µm², n=103 (Day 0, at Rest, No PBM) to 111.396±37.2 µm², n = 106 (Day 0, Post-6'WT, No PBM). That difference, an increase of 23.2 µm², or 26.3%, was statistically highly significant by two-tailed Student's t-test (t = -5.0335; df = 207; p<0.0001).
An aside: This result is quite different from that in Normal Controls, where the same exercise reduces neutrophil cell size in circulating cells.
Another aside: There are also some differences in distribution of "active" versus "resting" neutrophil cell membrane morphology or shapes in these same cell samples. Not to add to the confusion here, that topic of "shapes" and "activity" level, is better left for this separate article.
But the result is important and available. And yes, LTC and NC results are different.
But what happens to that "exercise effect" after PBM ?
In LTC subjects, AFTER any PBM, Head Only & Head and Back combined (Day 11 at rest, then 6 minute walking test)
Results now reflecting PBM and any exercise effects: Mean Neutrophil Size pre 6'WT
133.57±28.9 µm², n = 105 (Day 11, Pre-6'WT, Post-PBM) and 152.42±43.84 µm², n=116 (Day 11, Post-6'WT, Post-PBM). That difference, an increase of 18.9 µm², or 14.1%, was statistically highly significant by two-tailed Student's t-test (t = -4.0123; df = 219; p<0.0001).
Here the results from above are starting to be duplicated. But just to keep things togther for easier reading, what about the comparison with Normal Controls ?
In NC (normal, or Non-COVID Control) subjects, exposing Head Only (so, 10 minutes/ day) x 10 days - before and after exercise
Results now reflecting PBM, and possibly, any exercise effects: Mean Neutrophil Size pre 6'WT
154.02±21.74 µm², n = 60 (A normal value for size, Day 11, Pre-6'WT, Post-PBM) and 119.18±29.9 µm², n=60 (Day 11, Post-6'WT, Post-PBM). That difference, a reduction in mean neutrophil size of 34.84µm², or -22.62%, was statistically highly significant by two-tailed Student's t-test (t = -7.2998; df = 118; p<0.0001). And as seen before 10 days of PBM in Controls in response to exercise, a reduction in circulating neutraphil mean size here, once again. And, opposite the findings above in LTC subjects.
-----
Without wanting to overstate the importance of the results just presented, it is especially pertinent to underscore the importance of neutrophils in the innate immune system, and not understate that.
Neutrophils are doing much, much more than just gobbling up some bacteria in your gums each time you brush your teeth.
So what is at times summarized as the "heterogeneous structural and functional" findings of neutrophils, should allow us to expect a much greater role in creating those differences found here between LTC and NC subjects: And as important, their response to modifications in their cellular energy levels implied by their physical changes from an intervention with PBM.
PBM in these Normal Controls did not change neutrophil size.
Exercise in Normal Controls, before or after 10 days of PBM, reduced the size of circulating neutrophils as measured on peripheral blood smears.
Did the demands in the tissues (mostly muscle one assumes) of even brief (6 minutes) moderate exercise, move larger and more active neutrophils out of the capillary, and into the tissues, as a "normal" response ?
The response to PBM ± exercise in LTC subject neutrophils was clearly different.
And the "demands in the tissues" certainly extends beyond just muscle, as exercise physiologists have often confirmed. (Hormonal, nerve, brain, metabolic changes, etc).
Terms like "Post-Exertional Malaise," "Brain Fog" and others, readily come to mind.
Here we've made many "Before and After" observations about fairly objective data. (It's hard to subjectively control the size and shapes of one's neutrophils).
But the result of "just feeling better" should not be minimized.
That too will be objectively presented elsewhere, very soon.
---------
"OK. I understand. Who's got the light?"
>>> Introduction to Neutrophil cell membrane shape changes
>>> Our neutrophil shape change results in NC and LTC subjects
Can neutrophil-related damage be moderated by other than PBM?
Here's one example that is pertinent:
>>> Lots of info about Colchicine
And another:
>>> Neutrophils and Multiple Sclerosis
Morphology in Neutrophils - brief intro
StudyLTCOVID.com
Thanks for visiting!
To translate this page, select your
language from the dropdown menu below:
Morphology in neutrophils.
The word morphology refers of course to shape. It’s the study of form.
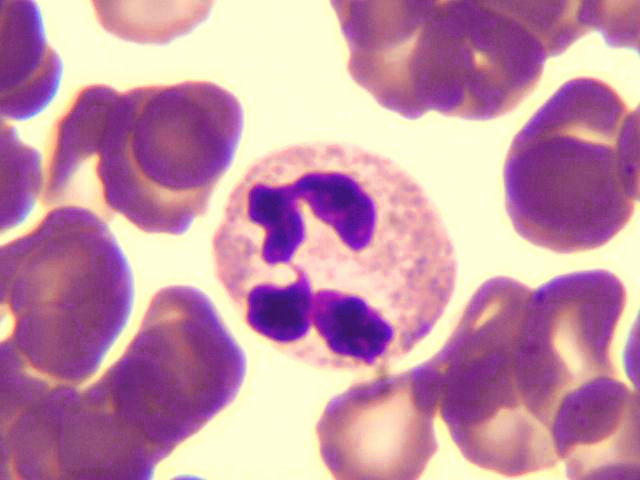
When applied to neutrophils, (about 50 to 70% of white blood cells) one can make observations about the shape of the central chromatin material, which seems to first attract the eye.
It can have many shapes. Hence the other name by which neutrophils are referred to: polymorphonuclear leukocytes (PMNs).
One can also make observations on the shape of a neutrophil’s cell membrane, which encloses not only the cell’s chromatin (DNA) but its several other components and granules. That's morphology too.
One may find neutrophils that appear on a peripheral blood smear as mostly round or spheroidal.
Others might be a bit more egg shaped, so ovoidal.
And again, others are perhaps larger at either end than in the middle, and stretched out a bit like an ellipse,
so, ellipsoidal.
Of course these cells all come from an individual subject. (Human or otherwise, but a subject with blood). And that subject has a clinical history which goes along with the individual. That "tale" can be related to standards for “perfect” or “normal” health. At times the history captures the findings in a disease process. And at other times, the possible effects of an intervention. Exercise might be one example. One can begin to imagine different such states: awake or asleep. Fasting or post-prandial. One easily imagines other comparisons of various bodily states of a subject, effects of medicines, etc. Elements defining a protocol for study if so desired.
COVID-19 ?
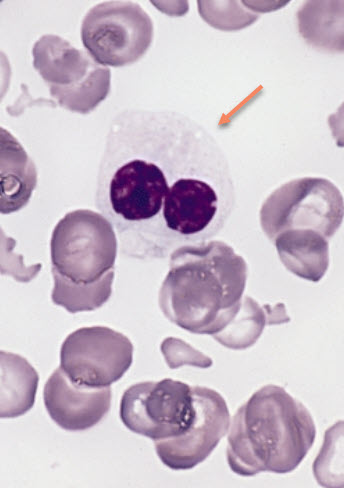
Specifically in COVID-19 positive subjects, several patterns of chromatin distribution or shapes have been described.
Terms have of course appeared to describe such findings, and their variation from what is considered normal. These can get lumped first under headings.
For example: anisocytosis: abnormalities of cell size. poikilocytosis: abnormalities or variations in cell shape. These are most often used to refer to changes in red blood cells. Nothing prevents one from applying these terms to a neutrophil.
Variations in PMN chromatin shape, and specifically in the setting of COVID-19, include descriptive terms like: “fetal or C-shaped chromatin,” “ring-shaped,” “elongated chromatin” as examples. Another complicated-sounding example: “Pseudo Pelger-Huët anomaly.” (And as seen below with its 'sunglasses' chromatin). Without explaining these or others in more detail, they are of course of use when observing a patient’s neutrophils microscopically. Other COVID-19 findings for other blood cells (lymphocytes, monocytes) could be presented, but let's stick to neutrophils.
Consistent with an expression like: “If it has feathers like a duck, walks like a duck, and quacks like a duck: it’s probably a duck,” The microscopic findings, applied systematically, can lead to moments that conclude with: ”... it’s probably COVID-19.” Imagine the potential utility when other tests have been negative, or a subject does not display the most often found set of historical and physical findings for COVID-19 and sequelae.
Almost a “Eureka!” moment in the lab.
And an equally important possible conclusion: "Nothing about what is seen on this peripheral smear, suggests COVID."
Let's close in a little
One can add to such information, another aspect of morphology: the shape of a neutrophil’s cell membrane. While not discussing that part of the cell in the detail that it certainly deserves, (and it still reserves many mysteries of structure, but especially function) here is one critical component: cellular energy supply and demand and related issues.
The use and maintenance of a cell’s membrane, is what demands the most energy of the cell. One can readily find examples of how a cell tries to adjust its membrane, to changes in available energy.
When one is driving one’s car on a trip, and the dashboard light is reminding that the vehicle is running on reserve sources of energy, and one is working through the distance to the next pump, one generally lifts one’s foot a bit and slows down. Neutrophils seem to do the same thing (haven’t observed one at the wheel of a vehicle so far). It would be logical if a neutrophil could still do its work with a smaller membrane circumference, when “on reserve.” (see an article on size results on this site, here) Related: one can easily find neutrophils budding off and ejecting pieces of its membrane, when the energy supply is low-ish.
Similarly, return of a “full tank” for neutrophils and their precursors in the marrow, might be associated to subsequent appearance of larger cells (anisocytotic (size) types of thoughts).
Do the shapes vary?
Can one observe pokilocytotic findings in the cell membranes of neutrophils: i.e., variations in the observed shape? Yes. That too has been reported previously.
If one wanted to try and push a beach ball through a keyhole (Good Luck!) it might be easier if you deflate the damn thing. Changing its shape would be an important contributor to the goal. (I have no suggestions about what to do with the damn thing, once on the other side).
Same for neutrophils.
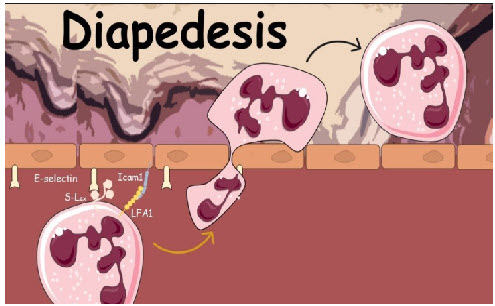
Their movement from “inside” the capillary to “outside” in the tissues includes a moment of squishiness and self-propelled push/ pull movement. That is called diapedesis. The cell membrane is more flexible: the clumped together chromatin probably less so. A neutrophil probably wants (shared with me in close personal discussions) to get its DNA through that tight space without breaking it to bits.
While neutrophils can manage this tight passage exodus just fine usually (when all the steps of the process are in order in the neutrophil AND in and between the capillary membrane cells), they are typically found rolling around in blood vessels in a spherical shape.
One might consider them in this state (and I’m imposing now on the visual observation), in readiness but not active. Or perhaps, less active. Yet, still available for a biochemical or biomolecular call to action. So, not completely on vacation.
The morphology that I call “ovoid,” is a transition state on the way to an “ellipsoid” shape. That latter is the required change for squeezing through.
These cell membrane morphology states represent a response to a “call” or change in biochemical environment. This might be locally (in endocrinology, referred to more recently as ‘paracrine’, like coming upon a wound or abscess in their travels). Or, in response to something dumped into their milieu - the circulating blood - by some unseen source, somewhere else. (Much more the original endocrine model). And it has become almost ‘de riguer’ in the populace to be able to recognize such “calls” to action (or inaction) in terms like: Interlekin-6 (pick another number if you like), Tumor Necrosis Factor, Platelet Activating Factor, and myriad others of course.
Can one match a neutrophil’s cell membrane morphology (shape), to whether it’s mostly resting, or busily changing its look to respond to action and get out there into the foray ?
Can the blend of shapes observed, lead to any conclusions of the energy state/ activity leve for the "team" (the n = ?) of neutrophils observed.
Well to forge ahead, this is exactly what I cautiously did.
I take neutrophils with a mostly spheroidal shape as inactive (or actually, less active, but ready for one of myriad possible calls).
I take neutrophils displaying an ovoidal shape as waking up, returning from vacation if you like, and accepting that “call to action” to get back to work.
And those with an “elliptical” morphology, as too busy with the response to even stop and talk a bit. They have lights and sirens going and they’re on their way to the blaze. Please step out of the way.
If one accepts any of that, and is willing to devote additional time to thinking about these tiny entities (13 or 14 microns in diameter in a light microscope. RBC’s average 7 microns), what might this imply ?
First: existence of an “in there” (capillary) and “out there” (tissues) set of environments. And since brain tissues and bone tissues (to pick two randomly) have some similarities but mostly differences, finding “parking” for oneself as one gets to the blaze may require a great deal of adaptability to various “scenes.” How one dresses when at home (capillary) might be quite different than one’s “look” when at a Birthday Party or a Funeral (tissues).
Secondly, if this notion of level of activity imposed on cell membrane morphology findings has any merit, how does it present or how does it vary in different “clinical settings” (to sound more like a physician than a fire fighter)?
Let’s next look at several such “clinical settings,” and see what we find.
Neutrophils will be categorized as “spheroidal,” “ovoidal,” and “ellipsoidal.” The ovoids and ellipses will be lumped together for counting. Those are taken as more active than the spheres, which will also be counted. Counts will also include percentages.
In categorizing observed neutrophils in this fashion, one should avoid judgements that a finding is "good" or "bad." If a blood smear (that's a sample from the circulation, so capillary side of things, not a tissue sample) shows very few neutrophils with an "active" morphology, maybe all of the "active" guys and gals are out in the tissues doing their job. To sample that, we'd need a biopsy.
Will these neutrophil cell membrane morphology findings prove to be the same in all settings, or variable ?
Final words of caution: finding what appear to be patterns or different mixes of morphology does not necessarily explain why that is so.
Finding changes in these observations on repeat sampling at different times, should include the fact that a neutrophils “life” once out of its formative infancy in the bone marrow, is quite short. Perhaps 18 to 36 hours. Some suggest some neutrophils live longer: 3 to 5 days. But those are outliers. Certain hypotheses have to fit the known facts, unless totally revolutionary and requiring throwing out, everything previously "known."
Which gets us to what or where ?
Last Final Word:
This is all about making observations, and learning from them.
For those living with "long-term" COVID-19 (LTC), such observations might be of interest.
But ultimately, if these findings can be linked to feeling better, they'd be happy I think.
I'd be happy, I'm sure.
As Louis Pasteur included in a speech one day: "Chance favors the prepared mind."
So let's continue the preparations, so Chance can move right in and finish the work.
In Surgery we used to say: "Better lucky than good," when it all worked out OK.
OK. With that introduction completed, back to the observations.
Neutrophil Cell Membrane SHAPE Observations
StudyLTCOVID.com
Thanks for visiting!
To translate this page, select your
language from the dropdown menu below:
Before presenting results below, getting a handle on the topic might be helpful.
Results, like in a published journal article, can get pretty dry pretty fast, if not placed in some context. Here is that introductory context. It can be read now or later of course. I put the same link at the bottom of this page.
A list for abbreviations you'll be seeing, is also at the bottom.
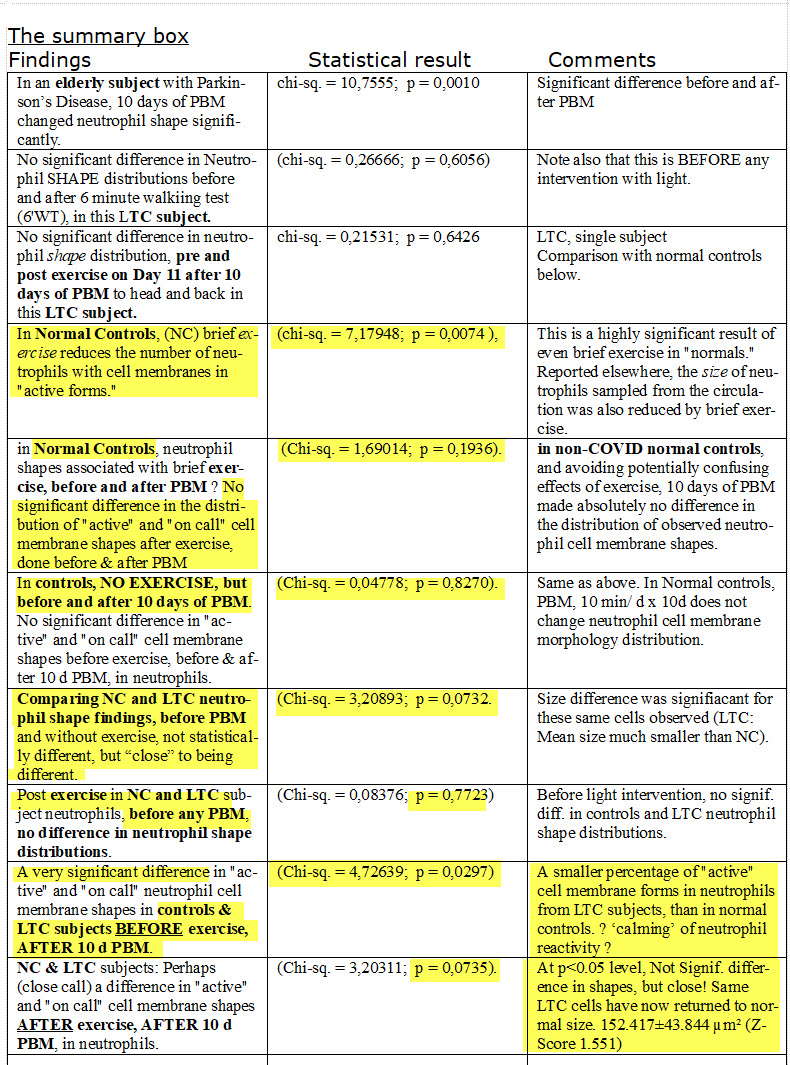
A Summary Box is present below. It summarizes all of the separate results sections. If your the kind of person who doesn't like living through the blow-by-blow stepwise process of the Scientific Method, ... you might have a look there right now.
But, no panic as you get into this! Just enjoy the view!
Sneaking up on the Results Observed
... first, some ungrouped observations (like a case presentation, but quicker !), followed by some more controlled comparisons.
---- 1 ----
A 79 year old man decides to get up on a chair outside in a light rain, to change a light bulb over his patio.
He falls.
A neighbor comes to the rescue. He falls too, breaking a few teeth of his dentures.
An ambulance is called and the 79 year old is seen in an ER. His neighbor goes home.
While in the ER, a test is positive for SARS-CoV-2. Nothing is broken. Skipping details of the ER story, he is sent home. (In my car at his wife's request. While at the hospital, I make a peripheral smear slide from his ER blood sample, fix it, stain it and look it over at my place, after getting him safely esconced at his home).
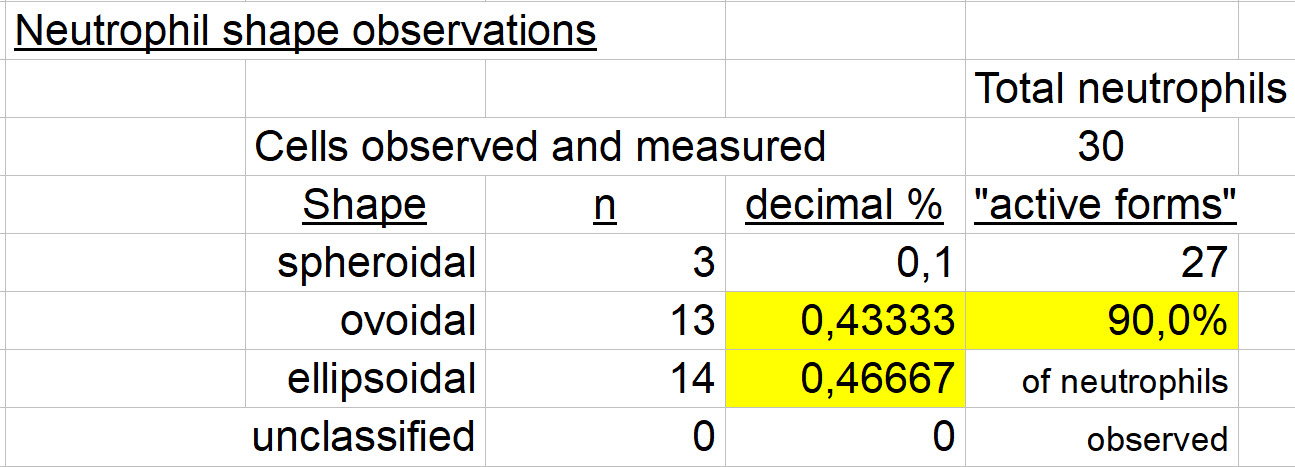
Below, the distribution of his neutrophil cell membrane findings:
I measured and qualified 30 of his neutrophils as to shape, as follows:
Cells that are "ovoidal" and "ellipsoidal" in form, have been highlighted and counted together.
That reflects a belief that they are more active forms of neutrophils, than the "spheroidal" cells. More on that hypothesis, below...
Setting: advanced age, acute mild trauma, an acute COVID-19 infection, (historically his second infection but no tests were done at that time). 90% of his circulating (intravascular) neutrophils are "active" shapes. One might postulate that to respond to an active coronavirus infection (and a little trauma too), one might like to see more "active forms" out in the tissues, leaving fewer to be observed in a sample from the circulation.
Maybe old people just do it that way.
---- 2 ----
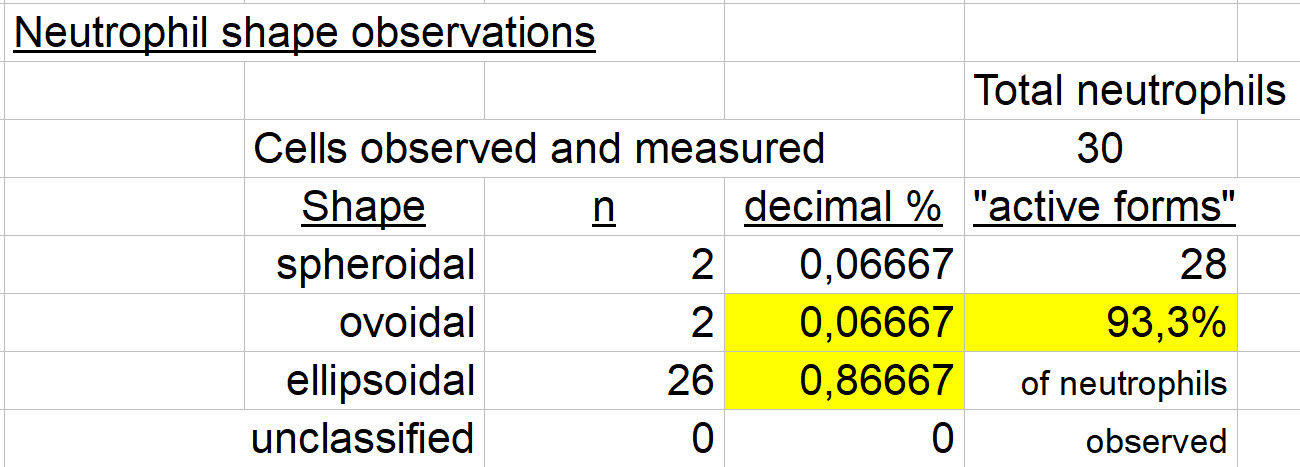
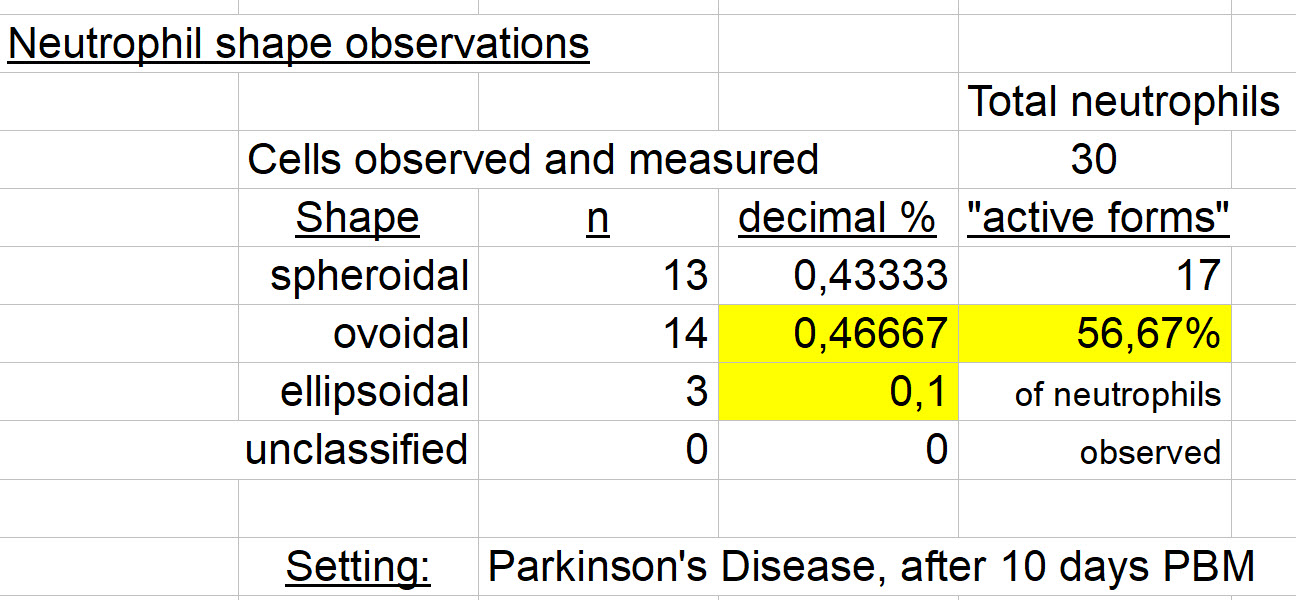
The spouse of the above subject; age 77. She has a history of Pakinson's Disease, treated with meds and a surgically implanted brain stem stimulator.
She has elected to try an intervention with light (photobiomodulation, PBM). Here below, results are from a blood sample before starting that intervention (Day 0).
An interesting aside: she and her husband have essentially identical results for the distribution of cell membrane morphologies (shapes). chi-sq. = 0,21818; p = 0,6404, means, no statistical difference.
Supposedly, no acute infection nor minor trauma in her case !
Are the findings related to advanced age? Hard to say. We continue with her results...
Below, results after 10 days of PBM to Head region, 10 minutes/ day.
Are the above results significantly different? : chi-sq. = 10,7555; p = 0,0010
So yes, very different in this single case.
After 10 days of PBM, there is a highly significant difference (reduction) of "active" neutrophil shaped cells in the circulation.
"Why ? We do not know." - quoting my Neuroanatomy Professor, Dr. Johnson in 1972.
Where did they go?
Perhaps out into various tissues of the body to respond to various "calls."
A bit more like "normal controls" as seen below.
Read on.
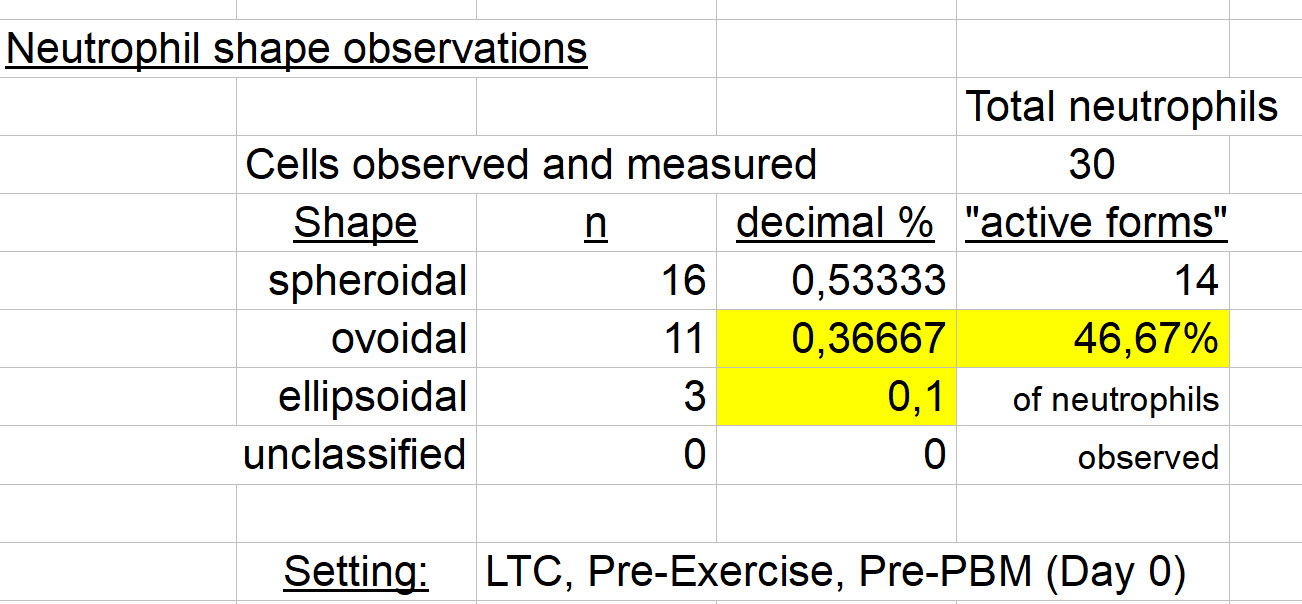
How about some LTC - related results ?
Okay. (Quick reminder: "LTC" = 'long-term' COVID-19)
Here's an LTC subject before any exercise, and before any PBM (Day 0). The mean neutrophil cell size of 65.282±15.374 sq.microns, is quite abnormally small (nl: 155-160 µm²).
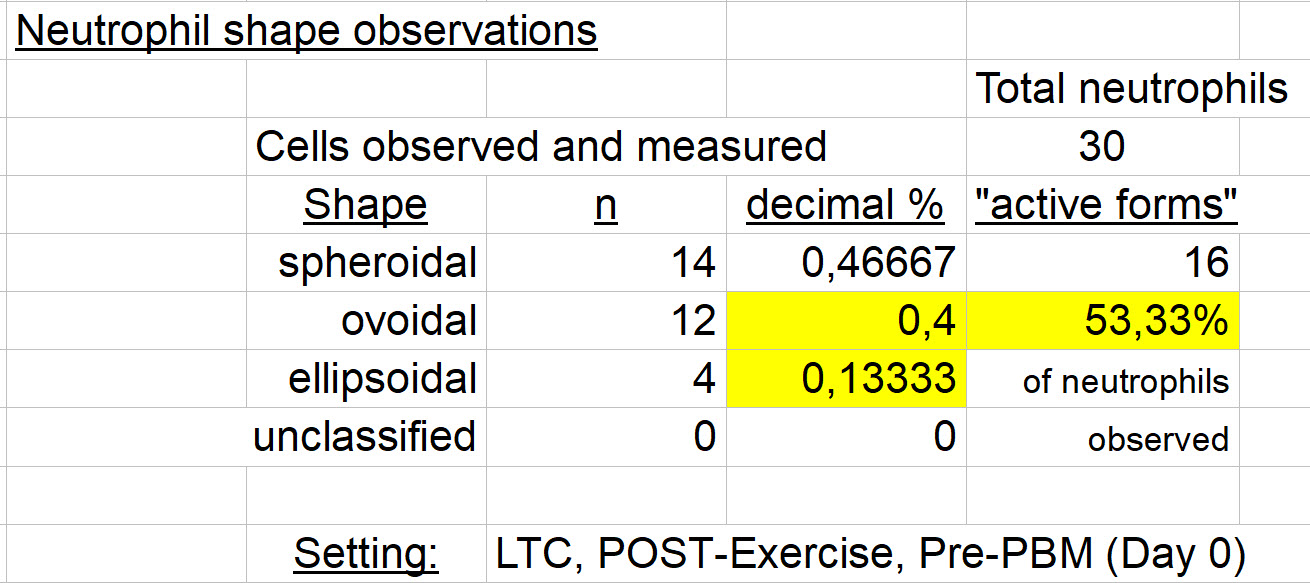
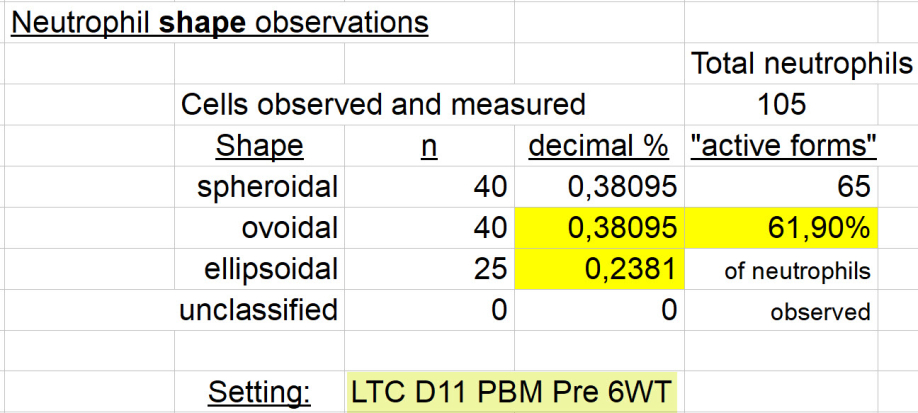
Next: Can one identify any effect of brief exercise (6 min. Walking Test) before PBM (Day 0) ?
(Cell size (area) has now increased to 91.808±18.769 µm², 15 min. after exercise. As noted elsewhere, circulating cell size after brief exercise diminishes in Normal Controls).
Interpretation: No significant difference in Neutrophil SHAPE distributions before and after a 6 minute walking test (6'WT).
(chi-sq. = 0,26666; p = 0,6056), in this LTC subject.
Note also that this is BEFORE any intervention with light.
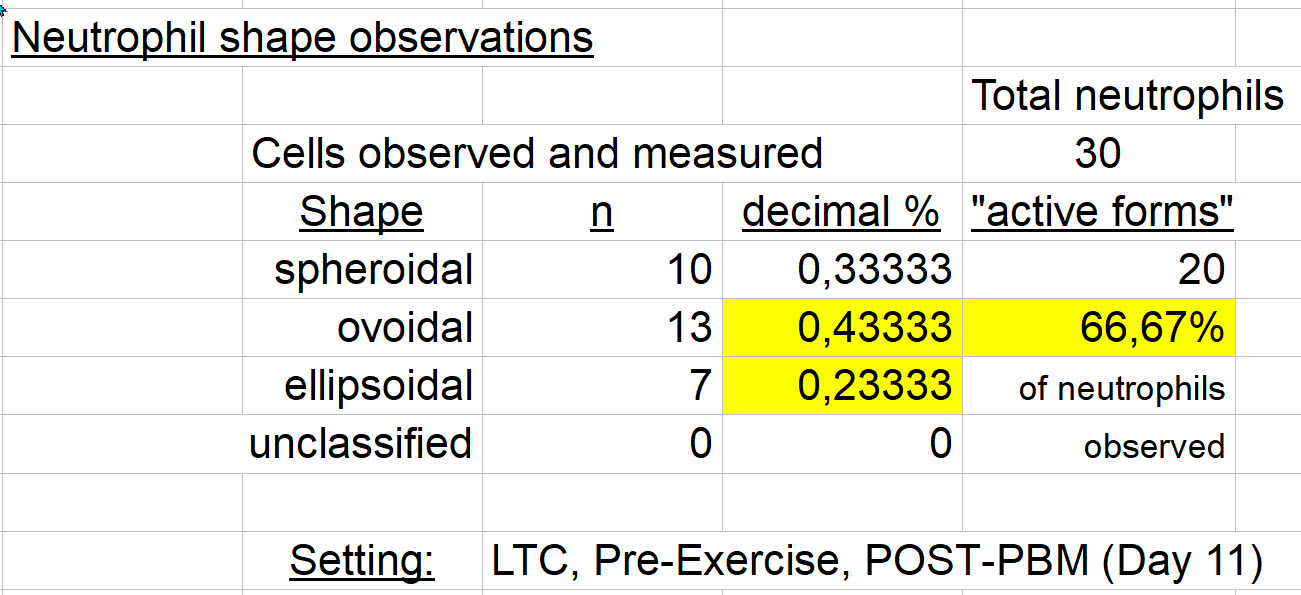
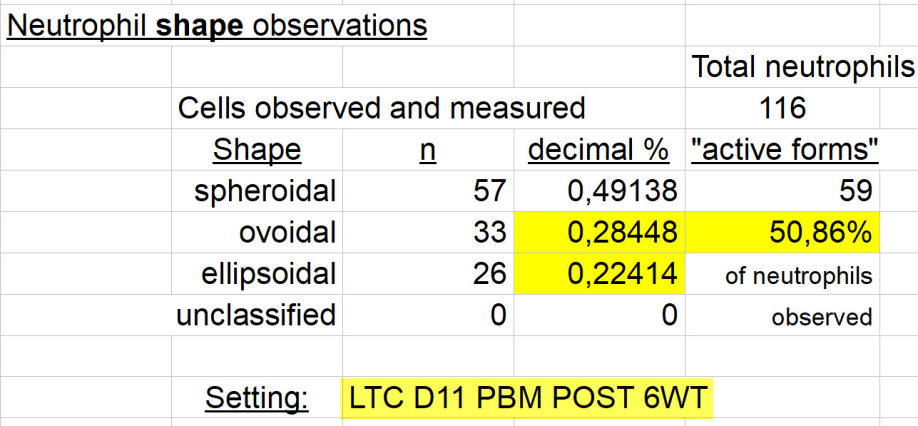
And after 10 days of PBM to head and back regions in LTC?
(Size (presented elsewhere) has increased to 111.202±19.277 µm². That's close to normal).
chi-sq. = 0,21531; p = 0,6426 So once again, no significant difference in neutrophil shape distribution, pre and post exercise on Day 11 after 10 days of PBM to head and back. Cell size increased significantly as just noted above. Putting that together: larger and more active forms of neutrophils in the vascular space, after an intervention with red and near-infrared light, in LTC.
Do the same neutrophils get out into the tissues more, or less ?
These data don't respond to that question.
Should one be anticipating a change in shape, either due to exercise, or to an intervention with light (PBM) ? What happens to cell membrane shape in Normal Controls ?
Normal Controls (NC) - Before 10 days of PBM and Before exercise (Day 0), compared with
After exercise on the same Day (0):
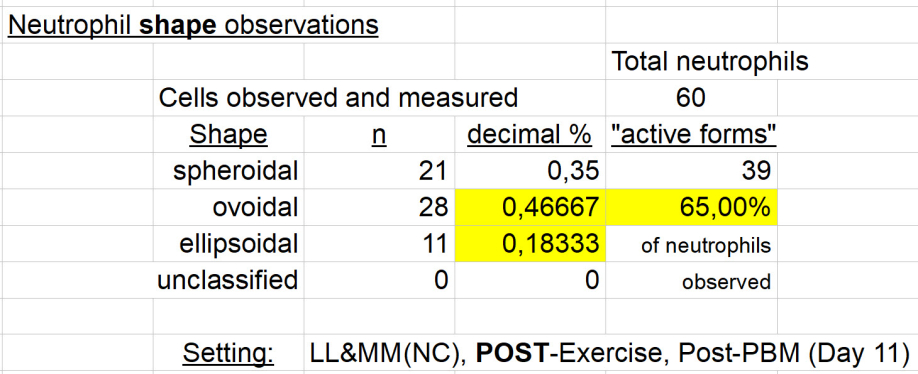
And now, after 10 days of PBM ...
Here below, Normal Controls, before exercise:
And here below, after exercise:
So are there differences in neutrophil cell membrane shape in normal controls, and if so, what is the impact of brief (6' walking test) exercise ? Are these results additionally modified after an intervention with photobiomodulation (PBM)?
A reminder, "active forms" represent the sum of neutrophils with ovoid and ellipsoid cell membranes. They can be further thought of as transitioning towards an exodus from the capillary (diapedesis) towards a call to action in the surrounding tissues.
Some comparisons, working towards answers to the above questions in these cells from Normal (non-COVID) Controls:
- Brief exercise reduces the number of neutrophils with cell membranes in "active forms." (chi-sq. = 7,17948; p = 0,0074 ), so this is a highly significant result of even brief exercise in "normals." Reported elsewhere, in this phase of the protocol, the size of neutrophils sampled from the circulation was also reduced by brief exercise. "Where did the 'big guys' go?"
- After 10 days of intervention with light, perhaps a difference in the distribution of "active" and "on call" (spheroidal) cell membrane shapes AFTER PBM, in neutrophils (p = 0,1051). While not statistically significant at the usual p<0.05 level, I interpret the values obtained here, as suggesting simply that something is going on. I.e., that there is a mixed effect of exercise and PBM on neutrophil shape in "normals." (Chi-sq. = 2,62653; p = 0,1051 ).
- How about, in Normal Controls, neutrophil shapes associated with brief exercise, before and after PBM ? No significant difference the distribution of "active" and "on call" cell membrane shapes after exercise, done before & after PBM (Chi-sq. = 1,69014; p = 0,1936).
- And in controls, NO EXERCISE, but before and after 10 days of PBM ? No significant difference in "active" and "on call" cell membrane shapes before exercise, before & after 10 d PBM, in neutrophils (Chi-sq. = 0,04778; p = 0,8270). So, in non-COVID normal controls, and avoiding potentially confusing effects of exercise, 10 days of PBM made absolutely no difference in the distribution of observed neutrophil cell membrane shapes, sampled from the circulation by fingerstick. (Just to say the same thing twice, for effect ! No judgements offered about "that's good!" or "that's bad!" It just is).
And when comparing results from those with LTC and these same values from Normal Controls ?
At the risk of sounding a little more scientific, the Null Hypothesis (Ho) states:
1. Pre exercise and pre intervention with light, no difference will be found in the distribution of "active" (Ovoidal and Ellipsoidal) and "on call" (Spheroidal) neutrophil shapes observed in Normal Controls (NC) and those with "long-term" COVID-19 (LTC):
Ho of 'no difference' is accepted. Chi-sq. = 3,20893; p = 0,0732.
But I'll tell you, ... p=0.07 is pretty damn close to being significant at the p<0.05 level, so the result it's trying to tell us something.
The neutrophil size difference looks like this for the same cells observed:
size = a mean area of 88.198±28.758 microns². That has a mean Z-Score of -2.938±2.818. The size for these LTC cells is about 3 standard deviations below the Mean for the Normal Controls. If that means nothing to you: very, very small, suggesting a low cellular energy state. A small cell membrane is easier to maintain than one of normal size, when one is 'running on reserve' as a neutrophil.
Summary: the LTC neutrophils are trending towards more active cell forms, and are definitely smaller neutrophils in the circulation, than those of normal controls.
Ho 2. Post exercise but still pre intervention with light, no difference will be found in the distribution of "active" (Ovoidal and Ellipsoidal) and "on call" (Spheroidal) neutrophil shapes observed in Normal Controls (NC) and those with "long-term" COVID-19 (LTC): 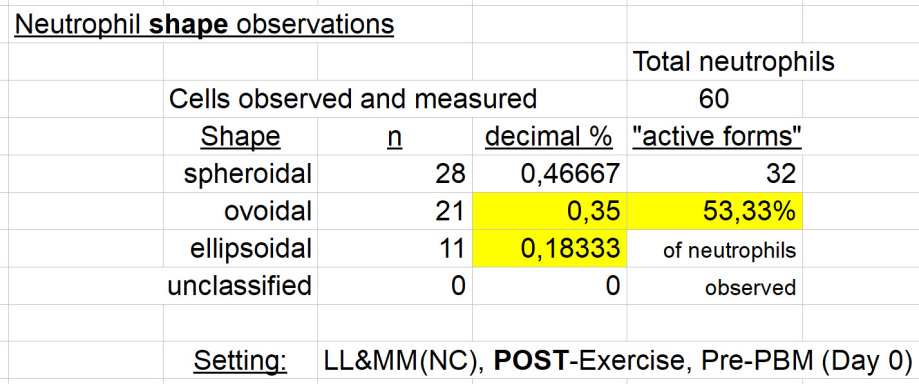
The null hypothesis (Ho) is sustained. No significant difference in the distribution of "active" and "on call" forms of neutrophil cell membranes. (Chi-sq. = 0,08376; p = 0,7723) from LTC subjects, when compared with those from controls.
A reminder: Mean cell size did increase in the LTC subjects (area = 111.395±37.200 µm²) which is still 1.3 standard deviations below normal size, for these 106 neutrophils observed.
Ho 3. Post 10 days PBM and pre exercise, no difference will be found in the distribution of "active" (Ovoidal and Ellipsoidal) and "on call" (Spheroidal) neutrophil shapes observed in Normal Controls (NC) and those with "long-term" COVID-19 (LTC): 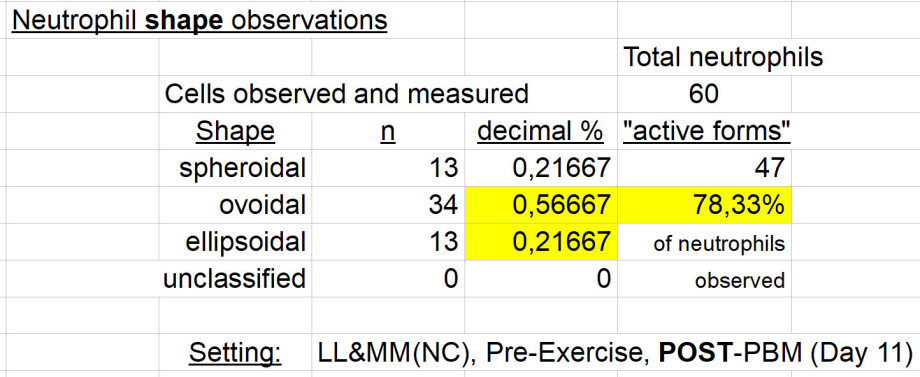
A very significant difference in "active" versus "on call" cell membrane shapes in controls & LTC subjects BEFORE exercise, AFTER 10 d PBM, in neutrophils (Chi-sq. = 4,72639; p = 0,0297). Null Hypothesis of no difference is rejected. A smaller percentage of "active" cell membrane forms in neutrophils from LTC subjects, than in normal controls.
To mention neutrophil size findings, the LTC mean neutrophil area of 133.566±28.883 µm², is essentially normal (Z-Score: 0.3690) after 10 days of PBM.
So, 10 days of PBM in LTC subjects gives results of normalized cell size, and
a circulating neutrophil cell membrane form that shows a difference (fewer active forms) from control values observed. It is conjecture to say that the PBM has "calmed" the level of reactivity of neutrophils in those with LTC, but there. I said it.
Other suggested interpretations are most welcome.
Ho 4. Post 10 days PBM and post exercise, no difference will be found in the distribution of "active" (Ovoidal and Ellipsoidal) and "on call" (Spheroidal) neutrophil shapes observed in Normal Controls (NC), compared with those with "long-term" COVID-19 (LTC):
Controls:
LTC subjects:
Perhaps a difference in "active" and "on call" cell membrane shapes AFTER exercise, AFTER 10 d PBM, in neutrophils (Chi-sq. = 3,20311; p = 0,0735).
One cannot reject the null hypothesis (Ho) of no difference, but again, one might say: "not quite statistically significant." If one develops a little bias, one can push an argument in either direction with such results.
Adding a final word on neutrophil size results here: The result is a Mean area of 152.417±43.844 µm². Well, that value is slightly above normal by Z-Score: 1.551. Call it normal size in neutrophils from LTC subjects, after 10 days of PBM.
Separating out effects of exercise and the intervention with light will require a bit more work to get closer to an understanding.
If one elects to stay quite clean with the statistical results, we have the following situation:
A Summary Table of Results
CONCLUSION
After 10 days of photobiomodulation in subjects with "long-term" COVID-19,
one can no longer find a difference in circulating neutrophil size nor in cell membrane form, when compared with cells from Normal Controls.
I rather like that as a conclusion.
And clearly, the results presented here include implications for further detailed study.
Certainly, this has raised more questions than it has answered.
For example:
- The first result at the top of this page. An elderly man, with an acute COVID-19 illness. Perhaps his second by history. His circulating neutrophils have an abnormal shape distribution, suggesting that they are in a very "active" state. Perhaps, even doing damage within his circulation. Is this finding:
- due to the acute infection ?
- due to his minor trauma (a fall, with nothing broken) hours before ?
- due to his advanced age ?
- his wife has similar findings, and a similar age
- but she has another illness, Parkinson's Disease
- due to something that is also going on in subjects with LTC ?
- they too have neutrophils circulating with a more "active" morphology
- perhaps pertinent, subjects with LTC have many parallels with effects of ageing, and as discussed in the article on this site.
One method for avoiding confusion in results, is to stay quite rigid in limiting subjects and their issues that are going to be studied.
Another method for avoiding confusion in sorting through these types of observations, is to stop making observations.
Surrendering the protocol.
Quitting.
---------
A.
Planning a protocol that investigates the potential effect(s) of an intervention, usually looks like this:
- Clean up the lab
- Find one single question to address
- Do a test, or some tests before, that answer that question
- Do the intervention
- Do the same tests after, as done before
- Make comparisons, validated by appropriate controls and statistical methods
- Explain and distribute what was observed
- So others can consider, compare, repeat, accept, refute, move forwards from there.
B.
Another approach is to simply ask participants if the intervention made them feel better.
That method seems valid for many.
The next participant may be embarking from a starting place that is not too different from the first participant, when this approach is applied.
It may be easier than the protocol method, which somewhere remains comitted to deciphering "the truth" about the question posed:
Identifying the message, without extraneous noise:
Reading the message correctly:
Approaching an understanding of what's next: deciding which port to sail towards.
---------
If one doesn't mind mixing a little "art" in the same cup with one's science, then read on...
---------
Neutrophils behave like tiny hand grenades. Once they get out into the tissues where cells of a tissue have put out a biochemical "call" for assistance, the neutrophil gobbles up the problem, sticks it in a little sac with poison called a vacuole, pulls the pin and explodes the bug or debris inside the sac. Or, it captures it with a NET, (a final parting gesture for the valiant neutrophil !); threrby preparing for its transport and disposal by macrophages or other cells.
But what would happen if, when a neutrophil gets the "call," it can't get out into the tissues, because the capillary wall has problems in those with LTC ?
Or perhaps it's the LTC neutrophil that has a problem with the capillary wall.
They just don't do this, like they loved to do before COVID ...
Then what ?
Well that sounds like a potentially quite farblunget (פארבלאנדזשעט) relationship and situation.
Well, perhaps these increasingly active forms before getting a little PBM, might still just "pull the pin." But wait ! What if they don't do that, out in a tissue with its current problem(s), but instead, in the circulation?
Somehow, a biochemical message to "pull the pin" made its way into the plasma from outside the circulation (called chemoattractants), and attached to one of the receptors on their smallish and energy-poor cell membrane, instantly changing their list of Things To Do. And from their, the usual quick, automatic, explosive response. Not enough energy left to think things over a bit, or waiting for the smoke or turbid plasma to clear: Reacting as usual like the body's Universal Soldier. Boom!
Yikes!
But if their toxic weapons get distributed in the circulation,... in the blood, and then carried around the body, ... perhaps that might cause a few problems.
Perhaps some readers can relate to that farblunget situation.
And for those who don't appreciate the hand grenade image, perhaps you'd prefer a sword.
If so, have a look here: Neutrophil chemoattractant receptors in health and disease: double-edged swords
In the article above, deep and up to date Science is clearly in support of our more imaginative possibilities for what neutrophils are capable of.
And from the above work:
"A chemoattractant gradient determines the direction of neutrophil migration. Activation of chemoattractant receptors induces the upregulation and activation of integrins. Binding of integrins to their ligands enables tight adhesion, eventually leading to trans- or paracellular migration. At the site of infection, neutrophils can phagocytose foreign material, including pathogens, produce reactive oxygen/nitrogen species (ROS/RNS) and release degradative enzymes and microbicidal agents (via degranulation) and neutrophil extracellular traps (NETs)."
Interesting (perhaps for some).
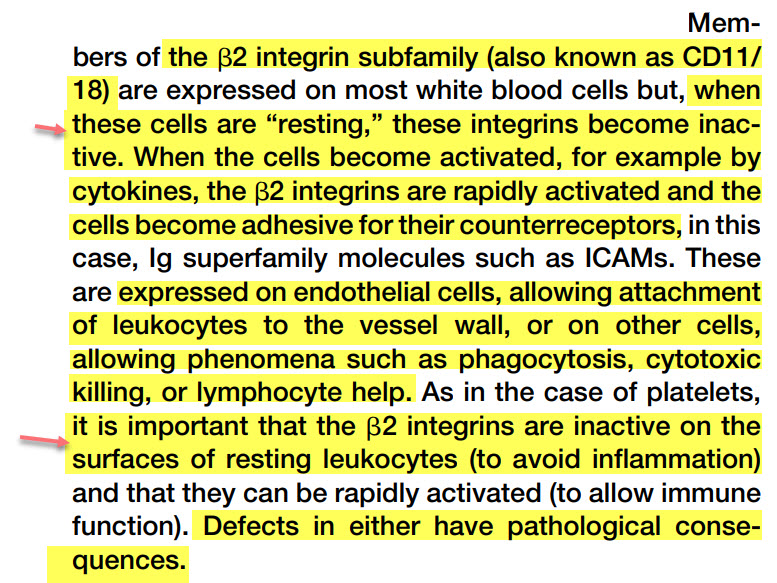
But do integrins have anything to do with SARS-CoV-2 infection and endothelial dysfunction, and as we've been exploring here in our results?
Why, sure they do ...
SARS-CoV-2 Spike triggers barrier dysfunction and vascular leak via integrins and TGF-β signaling
Integrins: Bidirectional, Allosteric Sgnaling Machines
Well, you get the idea.
Could one find a way to just calm these neutrophils down, just a bit ?
"Just a bit" is an important addition. Calm them down too much, and you might be supportive of a pneumonia, or wounds that don't heal.
One example of getting neutrophils to chill out just a bit: colchicine.
---------
"OK. I understand. Who's got the light?"
To other neutrophil articles on this site:
Neutrophil size observations >>>
Morphology in Neutrophils (if not read before) >>>
Neutrophils (several articles to help get over simplistic beliefs) >>>
Can neutrophil-related damage be moderated by other than PBM?
Here's one example that is pertinent:
>>> Lots of info about Colchicine
And another:
>>> Neutrophils and Multiple Sclerosis
List of abbreviations:
NC - Normal Controls
LTC - Long Term COVID
D0 - Day 0 (day of entry into study; before any intervention with light)
D11 - Day 11 (after 10 days of intervention. Usually with light, but in some controls may simply be an interval of time with nothing else.
PBM - photobiomodulation - an intervention with light of wavelength 660 to 670 nm (red), AND 830 to 850 nm (near-infrared) at a desired dose of 40 Joules/ cm².
No PBM - specifically, no light applied for these values obtained (could be applied later for other values presented elsewhere)
Pre 6WT - before a 6 minute walking test. Essentially at rest.
Post 6WT - after a 6 minute walking test. The sample of blood obtained, is as close to immediately after exercise as possible. The two samples (Pre- and Post- are typically 15 minutes apart.
Different Study ID#’s may also appear, and used to identify sample source.
examples: QIc-CM-1979, QI-AJW-1981, QI*OI-MD
They help to group samples logically by individual source identification, different arms of the study, presence of other illnesses, controls, etc.
Spher - spheroidal shape of cell membrane - might be thought of as in a “ready to respond” state, but still rolling around thinking of the last vacation.
Ov & Ellip - ovoid and ellipsoid shape of cell membrane. - might be thought of as “active forms.” They have initiated the response process. I think of them as a hand grenade, with its pin pulled, awaiting being thrown into action. Hopefully in a safe place for the other soldiers on our side.
Funding. No funding or sponsorship was
received for this study or publication of this
article.
That's not exactly right. The author took the hit completely, for all related expenses, and
of which there were quite a few. Money well spent. Some may disagree.