Measuring Vital Signs - why, what, when, how, and with what?
StudyLTCOVID.com
Thanks for visiting!
To translate this page, select your
language from the dropdown menu below:
Certainly arising out of habits developed during years of clinical practice, what we and others call "vital signs" are an essential part of this study, and are included in measurements to be made by each enrollee.
These are not "high-powered" immunologic tests carried out in a specialized lab or other hospital department.
But at times, when the "high-powered" tests returned mute, vital signs have tipped us off that something important was going on. They're in this protocol for no other reason. They must be treated with respect, and a devotion to making these measurements correctly. This site provides DEMO videos and explanations to make sure obtained results are valid.
I once saw a Nurse in ICU noting blood pressure measurements from an arterial line that had fallen out of the patient's wrist and was being banged by a ventilator with each provided breath to offer its data. Results were interesting. No immediate change was made in therapy.
Why?
When these measurements go on, day after day, and are found to be invariably normal, that may be less interesting, but still essential.
Many persons with "long-term" COVID-19 have obtained and used a pulse oximeter to measure peripheral oxygen saturation. The numbers are more than just a "good" or a "bad" result. Results in between, when repeated over time, may instruct quite a bit more.
That is just one example. But it represents an objective measure, if done correctly, and not just a subjective opinion about how one is breathing. That subjective opinion is important. Having the number to go along with that opinion is a value that one can work with. One can follow trends and calculate and compare averages to name a few things to do with data.
Measuring a person's temperature merits at least one comment. In the setting of "long-term" COVID-19, having a normal temperature may not be unusual. But the reason to measure is not to confirm what we already know. Instead, it is to wager on the possibilty of learning something that we did not know, and especially in the setting of an intervention under study.
What?
Meaning, what will be measured?
Weight and height at the start of the study. Weight again at the end. We assume height won't change much.
We'll use the metric system in all of this measuring, so Kilograms (Kg) and Centimeters (cm) are preferred.
If using a different system (like Stones for weight), we'll convert to metric.
Blood pressure (systolic and diastolic values), Heart rate or pulse (beats per minute or bpm), Peripheral Oxygen Saturation (%Sat), and Temperature (°C) will be measured daily for the duration of the study.
When?
On some days, Day 1 for instance, the measurements will be repeated at rest, then at 0, 5 and 10 minutes after a very mild walking exercise (as tolerated). Same at the end of the study.
But on most days, BP, HR, %Sat, Temp. Getting these basic measurements, quickly but accurately done (we'll help with that), is essential to finding differences due to light interventions, if these exist.
In the setting of a person following daily values, it is often recommended to make measurements at the same time each day, and in the same position. That may be applicable here as well. Every day, at 10AM for instance. Or if impractical, soon after arising.
Participants will receive specific instructions about these measurements, day by day during the study.
Here is a video overview for Vital Signs on different days of the study ...
How?
These measurements will be made in participant's homes.
To assure accurate and reproducible measurements, all participants will be using the same equipment. Provided to participants at no cost to them.
How to use each piece of equipment will be completely reviewed.
Also, how not to use it.
For instance, measuring Blood Pressure.
We get used to this being done in the office while seated, with a cuff on the upper arm. It's placed there, to be at heart level.
So if the supplied devices are placed on top of your head or in a pants pocket during measurements, you'll get a number. But not one of much value. We've figured that out.
We've made comparison measurements with standard practice columns of mercury sphygmomanometers (BP cuffs). We'll help you make your measurements at the right level.
One other practice. To avoid data loss, participants will send in daily measurements during the study via an email address: Vitals@StudyLTCovid.com
An UPDATE ...
EVEN BETTER!
There is now an online survey for reporting Vital Signs. Quite easy and fast!
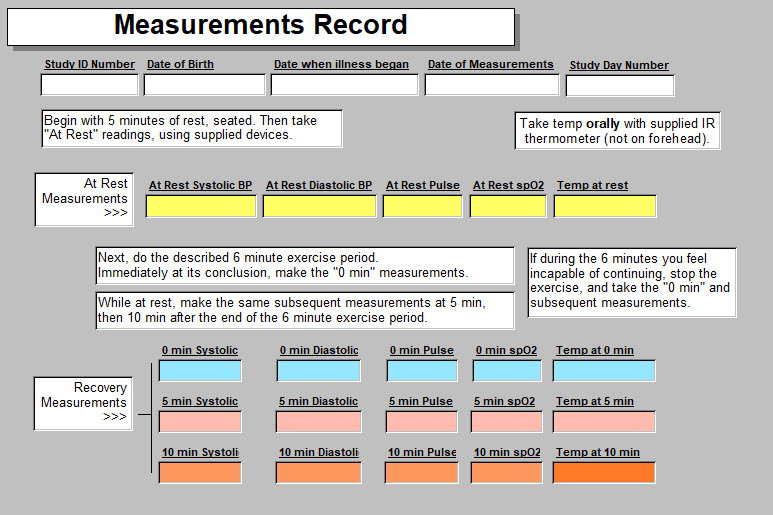
A form is supplied for participants to simplify jotting down the numbers. It might vary a bit from one arm of the study to the other, so may not look exactly like this but pretty close.
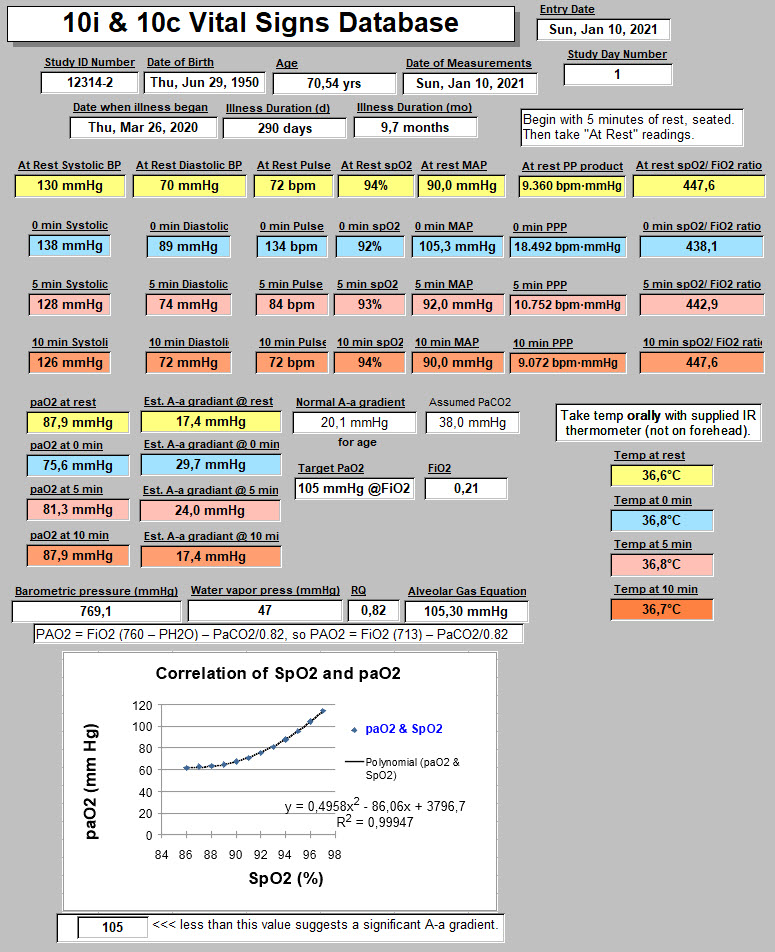
The person responsible for data entry and storage will place your results in a database, protecting all of your hard work.
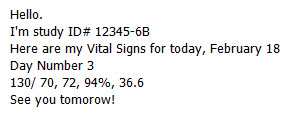
So sending off a quick email on any given study day might look like this:
Your result will not go to the Principal Investigator of the study while it's ongoing.
As part of the blinding process for this study, he won't see them until the end of data gathering. Notice that there is nothing to identify you personally besides the number you were assigned during the randomization at the start of the study.
But if your values are quite out of the norm, limits preset for the data-entry person, the Principal Investigator will be informed and you'll get a reply to see your personal physician and why. Not very likely, but that protects you.
But usually, your values will go into a database, and used to calculate other variables, and protected/ saved/ backed-up, to avoid data loss. That looks mostly like this:
With What?
As mentioned, the tools required for all physical measurements are provided.
Batteries too. ("What a deal!").
Even more than that, shipping expenses are covered.
Each has been checked to confirm normal function.
Even more than that, they have been checked for accuracy by simultaneous measurements made with equipment used in an ICU setting.
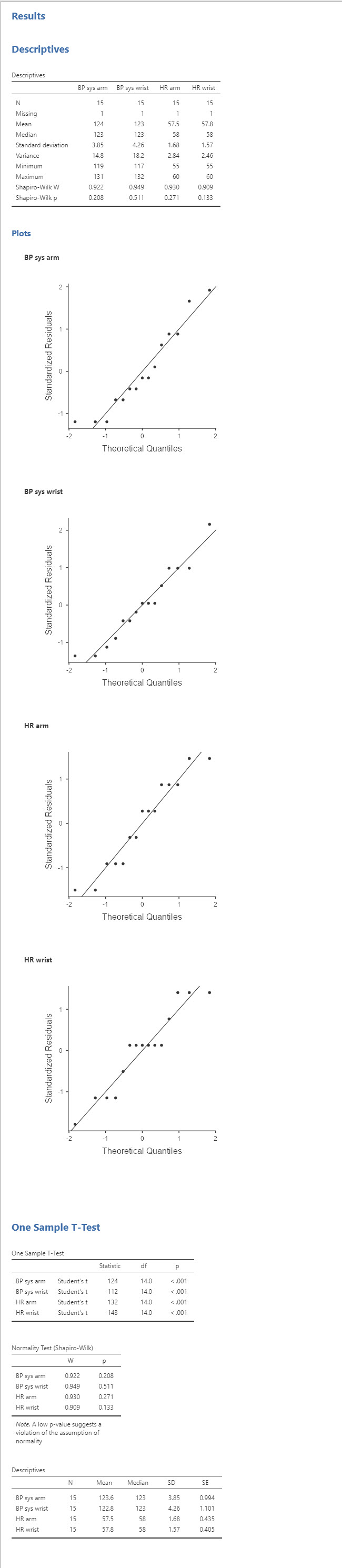
That leads to comparison data like this below. Rather boring but important to have.
The results below are just a sample of these comparisons.
Any time you see a p-value < 0.001, you're good to go!
So this was written to underscore the importance of having some objective measures of effect (or absence thereof!) for these lights in the "long-term" COVID-19 setting.
This study includes other objective measurements, and also some more subjective information and measurements of change over time. More on all that elsewhere, and especially when results are available.
<<<< Home